预约演示
更新于:2025-06-21
Gonyautoxin 2/Gonyautoxin 3
更新于:2025-06-21
概要
基本信息
药物类型 小分子化药 |
别名 Gonyautoxin 2/3、GTX 2/3、NAVX-010 |
靶点 |
作用方式 阻滞剂 |
作用机制 电压门控钠离子通道阻滞剂 |
治疗领域- |
在研适应症- |
非在研适应症- |
原研机构 |
在研机构- |
非在研机构 |
权益机构- |
最高研发阶段无进展临床1/2期 |
首次获批日期- |
最高研发阶段(中国)- |
特殊审评- |
登录后查看时间轴
结构/序列
分子式C10H17N7O8S |
InChIKeyARSXTTJGWGCRRR-LJRZAWCWSA-N |
CAS号60537-65-7 |
查看全部结构式(2)
关联
2
项与 Gonyautoxin 2/Gonyautoxin 3 相关的临床试验NCT04799041
Gonyautoxin 2/3 in the Treatment of Acute Back Pain (Study No CLN 17-032): A Clinical Proof-of-concept Study
This was an interventional, double-blind, placebo controlled, randomized, single dose, proof-of-concept study. It was a single-center clinical trial.
The purpose of the study was to explore the clinical efficacy and safety of a single local IM injection of gonyautoxin 2/3 (GTX 2/3) compared to placebo in decreasing pain and improving lumbar functionality at short term follow-up in adult patients with acute low back pain, without radiculopathy.
The purpose of the study was to explore the clinical efficacy and safety of a single local IM injection of gonyautoxin 2/3 (GTX 2/3) compared to placebo in decreasing pain and improving lumbar functionality at short term follow-up in adult patients with acute low back pain, without radiculopathy.
开始日期2019-10-11 |
申办/合作机构 |
NCT03655522
NAVX-010 - A Phase I, Double-Blind, Placebo-Controlled, Single-Dose, Safety, Tolerability and Pharmacokinetic Study in Healthy Male Subjects
This was a double-blind, placebo-controlled, randomized, single ascending dose, sequential group study. Each subject participated in only 1 treatment period.
The primary objective was to determine the safety of single intramuscular (IM) injections of NAVX 010 in healthy subjects. The secondary objective was to determine the single dose pharmacokinetics (PK) of Gonyautoxin 2 (GTX 2) and Gonyautoxin 3 (GTX 3) following IM administration of NAVX 010 in healthy subjects.
Thirty subjects were studied in 5 groups (Groups A to E); each group consisted of 6 subjects, of which 4 subjects received the Investigational Medicinal Product and 2 subjects received placebo. All subjects completed the study and data for all subjects were included in the safety analyses. A total of 20 subjects received NAVX-010 and were included in the PK population and subsequent PK analysis.
The primary objective was to determine the safety of single intramuscular (IM) injections of NAVX 010 in healthy subjects. The secondary objective was to determine the single dose pharmacokinetics (PK) of Gonyautoxin 2 (GTX 2) and Gonyautoxin 3 (GTX 3) following IM administration of NAVX 010 in healthy subjects.
Thirty subjects were studied in 5 groups (Groups A to E); each group consisted of 6 subjects, of which 4 subjects received the Investigational Medicinal Product and 2 subjects received placebo. All subjects completed the study and data for all subjects were included in the safety analyses. A total of 20 subjects received NAVX-010 and were included in the PK population and subsequent PK analysis.
开始日期2015-05-14 |
申办/合作机构  Algenis SpA Algenis SpA [+1] |
100 项与 Gonyautoxin 2/Gonyautoxin 3 相关的临床结果
登录后查看更多信息
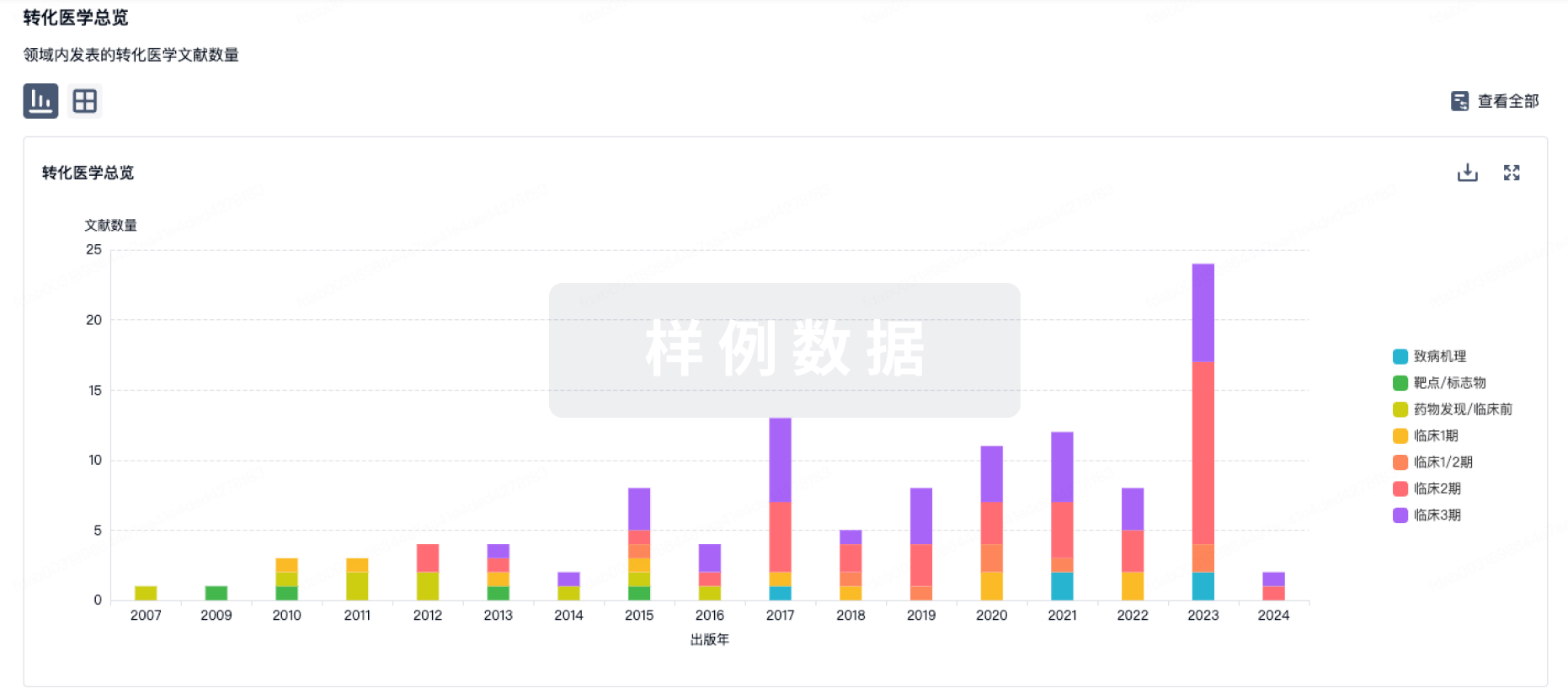
100 项与 Gonyautoxin 2/Gonyautoxin 3 相关的转化医学
登录后查看更多信息
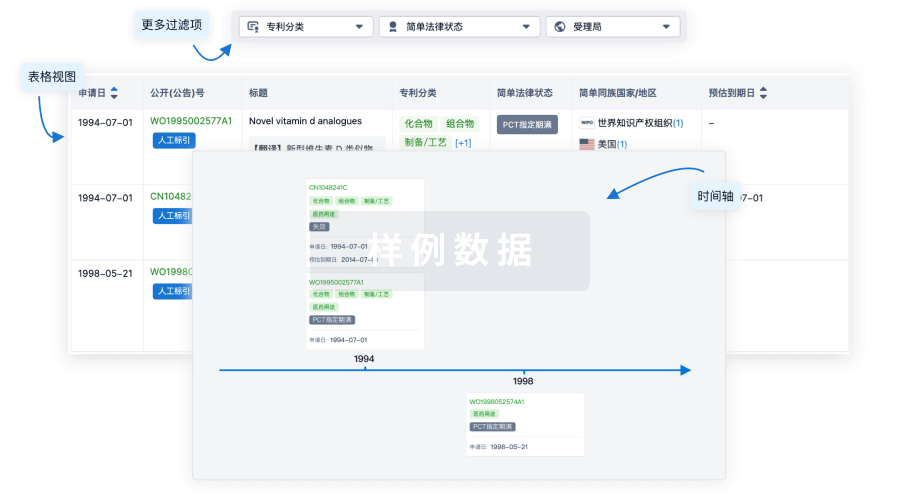
100 项与 Gonyautoxin 2/Gonyautoxin 3 相关的专利(医药)
登录后查看更多信息
6
项与 Gonyautoxin 2/Gonyautoxin 3 相关的文献(医药)2023-03-01·The journal of knee surgery4区 · 医学
Gonyautoxins 2/3 Local Periarticular Injection for Pain Management after Total Knee Arthroplasty: A Double-Blind, Randomized Study
4区 · 医学
Article
作者: Hinzpeter, Jaime ; Lagos, Néstor ; Barahona, Maximiliano ; Palet, Miguel ; Aliste, Julián ; Catalan, Jaime ; Zamorano, Alvaro ; Campo, Miguel del ; Barrientos, Cristian
Abstract:
The purpose of this study was to compare the efficacy of periarticular infiltration of gonyautoxin 2/3 (GTX 2/3) and a mixture of levobupivacaine, ketorolac, and epinephrine for pain management after total knee arthroplasty (TKA). Forty-eight patients were randomly allocated to receive periarticular infiltration of 40 µg GTX 2/3 (n = 24) diluted in 30 mL of sodium chloride 0.9% (study group) or a combination of 300 mg of levobupivacaine, 1 mg of epinephrine, and 60 mg ketorolac (n = 24) diluted in 150 mL of sodium chloride 0.9% (control group). Intraoperative anesthetic and surgical techniques were identical for both groups. Postoperatively, all patients received patient-controlled analgesia (morphine bolus of 1 mg; lockout interval of 8 minutes), acetaminophen, and ketoprofen for 72 hours. A blinded investigator recorded morphine consumption, which was the primary outcome. Also, the range of motion (ROM) and static and dynamic pain were assessed at 6, 12, 36, and 60 hours after surgery. The incidence of adverse events, time to readiness for discharge, and length of hospital stay were also recorded. The median of total cumulative morphine consumption was 16 mg (range, 0–62 mg) in the GTX 2/3 group and 9 mg (range, 0–54 mg) in control group, which did not reach statistical difference (median test, p = 0.40). Furthermore, static and dynamic pain scores were similar at all time intervals. GTX 2/3 was inferior in range of motion at 6 and 12 hours; nevertheless, we noted no difference after 36 hours. No differences between groups were found in terms of complications, side effects, or length of hospital stay. No significant differences were found between groups in terms of breakthrough morphine requirement. However, local anesthetic use resulted in an increased ROM in the first 12 hours. This prospective randomized clinical trial shows that GTX 2/3 is a safe and efficient drug for pain control after TKA; nevertheless, more studies using GTX 2/3 with larger populations are needed to confirm the safety profile and efficiency. This is level 1 therapeutic study, randomized, double-blind clinical trial.
2013-06-01·Toxicon : official journal of the International Society on Toxinology3区 · 医学
A novel method for preparing complete antigens of gonyautoxin 2,3 and their feature of immunogenicity
3区 · 医学
Article
作者: Huajuan Lin ; Rui Zhang ; Xiaoming Qin ; Caohua Zhang ; XiHong Yang ; YunTao Zhao
In this paper, a novel method was proposed to prepare artificial antigens of gonyaulax parlaytic shellfish toxin 2 and 3 (GTX2,3). An intermediate GTX2,3-aldehyde was first synthesized by activating the NH₂ group of the 2nd and 8th amino acid residues with three different aldehydes and two artificial complete antigens GTX2,3-aldehyde-bovine serum albumin (BSA) and GTX2,3-aldehyde- keyhole limpet hemocyanin (KLH) were then prepared by cross-linking the intermediate with BSA or KLH. The successful preparation of the two complete antigens was confirmed by UV spectral scanning, HPLC, production of antibodies with titer of 1.28 × 10⁴ from mice immunized with the two complete antigens, indirect ELISA and Western-blot. In conclusion, the synthesized complete antigens have strong immunogenicity, which provides a solid foundation for preparing GTX2,3 monoclonal antibody and rapid detection kit.
2010-01-01·Analytica chimica acta2区 · 化学
A sensitive immunosorbent bio-barcode assay combining PCR with icELISA for detection of gonyautoxin 2/3
2区 · 化学
Article
作者: Wenfei He ; Junjian Xiang ; Hong Wang ; Yaoqiang Chen ; Yong Tang ; Ning Deng ; Hongyu Yang
In the current study, we developed a nanosphere bio-barcode technology to detect trace gonyautoxin 2/3 (GTX 2/3). GTX 2/3-glucose oxidase (GOX) conjugates were first prepared as the coating antigen in a periodate reaction. Subsequently, gold nanoparticles (NP) dual-labeled with anti-GTX 2/3 monoclonal antibodies (Mab) and DNA oligonucleotides were synthesized via a one-step preparation method. Combining PCR with indirect competitive ELISA (icELISA), a novel immunosorbent bio-barcode assay was established utilizing the Mab-NP-dsDNA complex to convert enzymatic signals to DNA signals. Importantly, the limit of detection of the method was lower than 0.74 microg mL(-1). Thus, the immunosorbent bio-barcode assay is a rapid and high-throughput screening tool to detect GTX 2/3 in aquatic products.
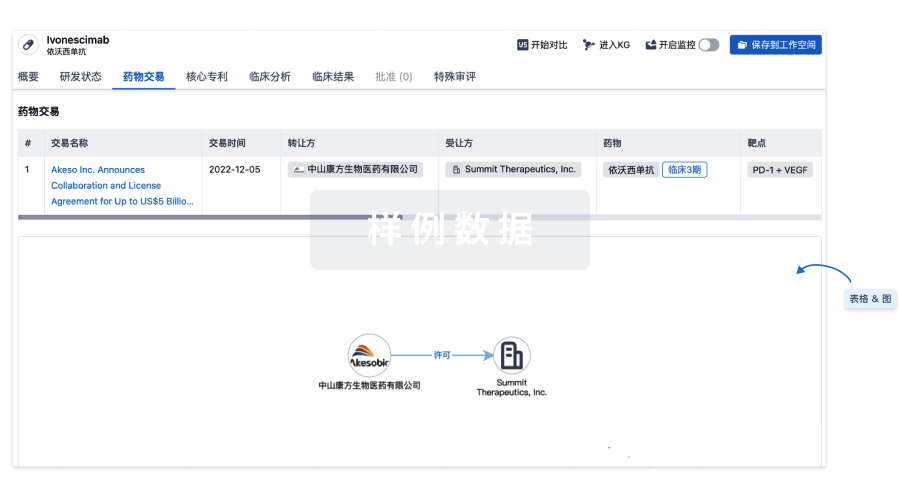
100 项与 Gonyautoxin 2/Gonyautoxin 3 相关的药物交易
登录后查看更多信息
研发状态
登录后查看更多信息
临床结果
临床结果
适应症
分期
评价
查看全部结果
| 研究 | 分期 | 人群特征 | 评价人数 | 分组 | 结果 | 评价 | 发布日期 |
|---|
No Data | |||||||
登录后查看更多信息
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
核心专利
使用我们的核心专利数据促进您的研究。
登录
或
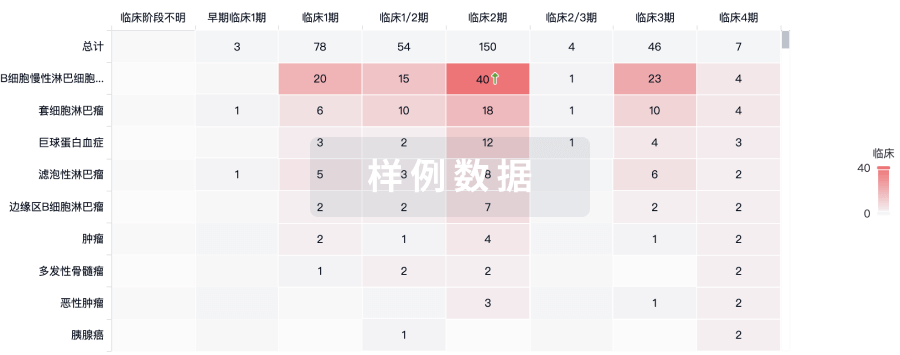
临床分析
紧跟全球注册中心的最新临床试验。
登录
或
批准
利用最新的监管批准信息加速您的研究。
登录
或

特殊审评
只需点击几下即可了解关键药物信息。
登录
或

Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用