预约演示
更新于:2025-06-07
Troleandomycin
醋竹桃霉素
更新于:2025-06-07
概要
基本信息
药物类型 小分子化药 |
别名 Oleandocetine、Oleandomycin triacetate、Oleandomycin triacetyl ester + [9] |
作用方式 抑制剂 |
作用机制 50S subunit抑制剂(50S核糖体亚基抑制剂) |
治疗领域 |
在研适应症- |
非在研适应症 |
在研机构- |
权益机构- |
最高研发阶段撤市 |
首次获批日期 美国 (1969-05-27), |
最高研发阶段(中国)- |
特殊审评- |
登录后查看时间轴
结构/序列
分子式C41H67NO15 |
InChIKeyLQCLVBQBTUVCEQ-QTFUVMRISA-N |
CAS号2751-09-9 |
关联
100 项与 醋竹桃霉素 相关的临床结果
登录后查看更多信息
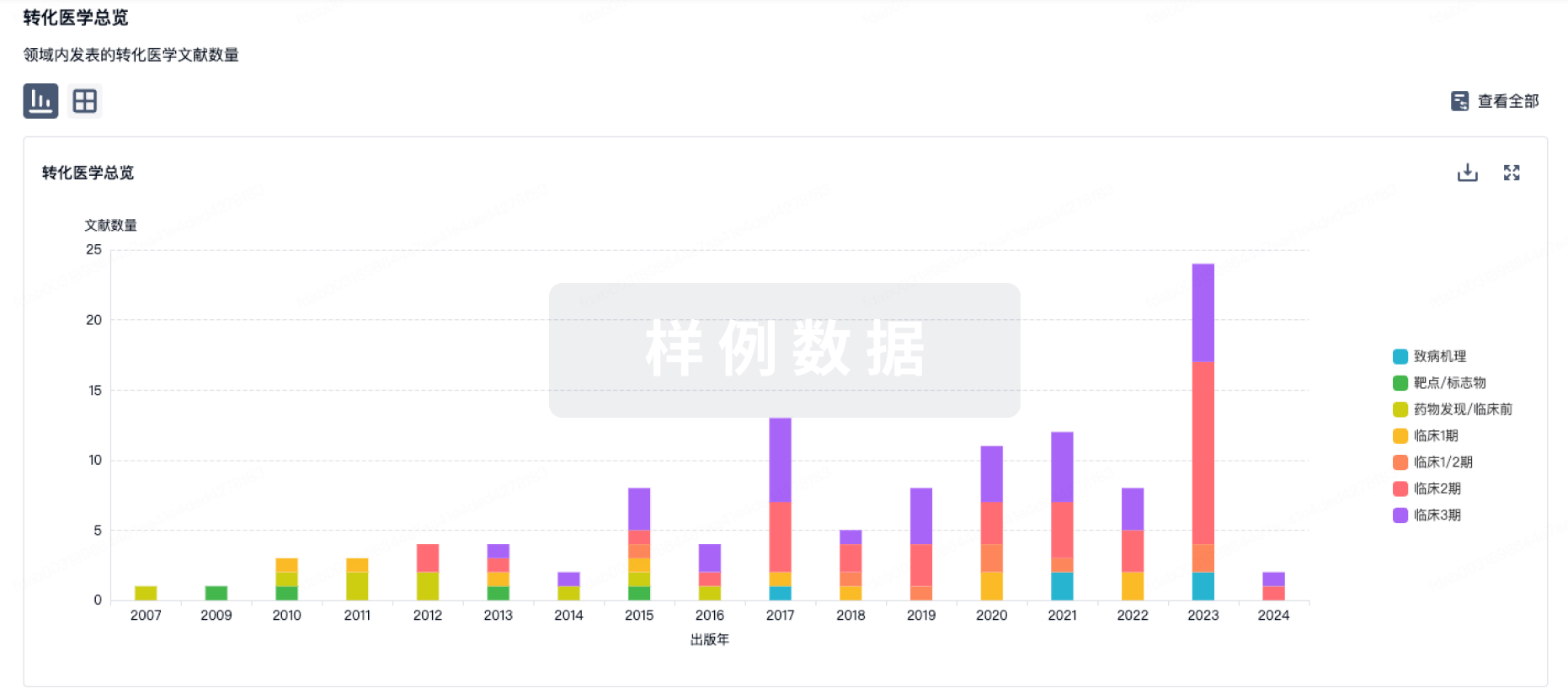
100 项与 醋竹桃霉素 相关的转化医学
登录后查看更多信息
100 项与 醋竹桃霉素 相关的专利(医药)
登录后查看更多信息
1,721
项与 醋竹桃霉素 相关的文献(医药)2025-07-01·JOURNAL OF SURGICAL RESEARCH
Trimethylamine N-Oxide and Smoking Are Associated With the Progression of Thromboangiitis Obliterans
Article
作者: Zou, Zhong-Hui ; Wang, Song ; Luo, Hong ; Wang, Min ; Pan, Zhong-Hui ; Zhang, Wen-Jing ; Su, Mei-Lan
INTRODUCTION:
Thromboangiitis obliterans (TAO) is potentially associated with smoking, although its precise pathogenesis remains unclear. Trimethylamine N-oxide (TMAO) has been implicated in the induction of various cardiovascular and cerebrovascular diseases. However, the role of TMAO in TAO has not been reported. This study aimed to investigate the relationship between smoking, TMAO, and TAO.
MATERIALS AND METHODS:
Thirty-three patients diagnosed with TAO and hospitalized for treatment between January 2018 and July 2024 were included in the study. Healthy smokers (n = 38) and nonsmokers (n = 35) were randomly recruited and matched for age, sex, and education level as controls. Subsequently, we analyzed their clinical characteristics, levels of TMAO, and immune and inflammatory markers.
RESULTS:
Patients with TAO exhibited significantly higher levels of TMAO, Toll-like receptor 4 (TLR4), receptor for advanced glycation end products, interleukin (IL)-1β, IL-18, tumor necrosis factor-alpha, high mobility group box 1, nuclear factor-κB (NF-κB), and phosphorylated NF-κB (pNF-κB) than those in the smoking and nonsmoking control groups (all P < 0.05). The smoking control group also exhibited significantly higher levels of TMAO, TLR4, IL-1β, NF-κB, and pNF-κB (all P < 0.05) than the nonsmoking control group. TMAO, IL-1β, and tumor necrosis factor-alpha levels were significantly higher in the underage smoking group (all P < 0.05) than in the adult smoking group. The level of TMAO was significantly correlated with the Rutherford classification in patients with TAO, patients' smoking status (including total years of smoking and average daily cigarette consumption), and immune and inflammatory markers (all P < 0.05).
CONCLUSIONS:
These findings indicate that gut microbiota plays a significant role in the pathogenesis of TAO. TMAO is likely involved in the pathogenesis and progression of TAO, with smoking acting as a contributing factor. The underlying mechanism may involve the activation of immune-inflammatory pathways, specifically the high mobility group box 1-receptor for advanced glycation end products/TLR4-NF-κB pathway.
2025-06-01·Brain Imaging and Behavior
Effect of glucocorticoid therapy on brain white matter microstructure in thyroid-associated ophthalmopathy: a longitudinal diffusion kurtosis imaging study.
Article
作者: Wu, Fei-Yun ; Zhou, Jiang ; Xu, Xiao-Quan ; Wu, Qian ; Pu, Xiong-Ying ; Chen, Huan-Huan ; Hu, Hao ; Lu, Jin-Ling
To investigate the changes in brain white matter microstructure in patients with thyroid-associated ophthalmopathy (TAO) before and after glucocorticoid therapy using diffusion kurtosis imaging (DKI) with tract-based spatial statistics (TBSS) method. Twenty TAO patients and 20 healthy controls were enrolled for clinical and magnetic resonance imaging (MRI) examinations. All patients had intravenous glucocorticoid therapy, followed by MRI scans and clinical assessments three months after the treatment ended. TBSS was used to evaluate the mean kurtosis (MK), axial kurtosis (AK), radial kurtosis (RK), kurtosis fractional anisotropy, fractional anisotropy (FA) and mean diffusion of brain white matter. At baseline, TAO patients showed significantly decreased MK, AK, RK and FA in extensive white matter tracts compared to controls. After therapy, increased MK and AK were observed in comparison to the pre-therapy cohort. However, post-therapy TAO patients still exhibited reduced RK in partial white matter tracts compared to controls. RK values in left posterior thalamic radiation (PTR) showed a negative correlation with CAS in pre-therapy TAO patients. Meanwhile, RK values in left PTR were positively correlated with quality of life scores for visual functioning, and RK values in left anterior corona radiata were negatively correlated with anxiety scores in post-therapy TAO patients. Our findings suggested that TAO could lead to white matter deficits in the visual, cognitive, and emotional brain areas, which were partially restored after treatment.
2025-05-01·Small
Cerium Nanozyme‐Powered Hydrogel Microspheres Alleviate Thromboangiitis Obliterans via Enhanced Stem Cell Therapy
Article
作者: Shafiq, Muhammad ; Liang, Xiao ; Lan, Zhengyi ; Shi, Zhangpeng ; Chen, Hangrong ; Ma, Ming ; Zhang, Yiqing ; Shu, Yimeng
Abstract:
Thromboangiitis obliterans (TAO) is a chronic peripheral vascular condition characterized by thrombotic and inflammatory acceleration. As a promising therapeutic modality for the TAO, mesenchymal stem cells (MSCs) transplantation is expected to circumvent the traditional drug therapy and surgical interventions. Nonetheless, the MSCs therapy is hindered owing to poor survival, retention, and engraftment of the transplanted cells. The objective of this research is to develop MSCs‐ and cerium oxide nanoparticles (CeNPs)‐laden injectable methacrylated gelatin (GelMA)‐based hydrogel microspheres by using microfluidics and discern their potential to regulate oxidative stress and inflammation in a rat model of TAO. The CeNPs‐loaded photocroslinkable GelMA microspheres not only protected the transplanted MSCs against oxidative stress but also facilitated endothelial functional recovery, revascularization of the ischemic limb, and suppression of the inflammatory factors from the macrophages. The hydrogel microspheres further conferred mechanical support and prolonged the residence time of transplanted MSCs to enhance the efficacy of cell therapy. In vivo study confirmed that the combination of MSCs and CeNPs in the microsphere exhibited a positive synergistic effect on tissue recovery and angiogenesis. Taken together, this work presents a novel therapeutic approach based on the integration of stem cells and nano‐micron combined hydrogel microspheres, which may have implications for TAO therapy.
9
项与 醋竹桃霉素 相关的新闻(医药)2023-12-13
·今日头条
编者按:
在现代养殖业中,饲用促生长抗生素(AGPs)的应用曾经是提高畜禽生长效率、促进饲料转化率的常见做法。然而,随着对抗生素抗药性问题认识的加深,这一做法已经引起了国际社会的广泛关注。抗生素抗药性不仅威胁到动物健康,更对人类健康构成间接风险,因为它可能通过食物链传递给人类,导致医疗抗生素的效力下降。鉴于此,许多国家和地区开始制定政策,限制或完全禁止在养殖业中使用促生长抗生素。
今天,我们共同关注禁抗与替抗问题。希望本文能够为相关的产业人士和诸位读者带来一些启发和帮助。
① 国外禁抗的发展历程
20世纪四十年代后期,四环素(抗生素的一种)首次被报道可能有饲用促进肉鸡生长的特性。四环素的这种促生长作用很快在其他抗菌剂和动物物种中被进一步证实,并被快速应用于工业化畜牧业生产系统中。在动物生产中,“饲用抗生素”是指低剂量(亚治疗剂量)长期应用于饲料中,以保障动物健康、促进动物生长与生产、提高饲料利用率的抗生素,也就是人们常说的饲用促生长抗生素(antibiotic growth promoters,AGPs)。
饲用抗生素的应用极大地促进了养殖业的蓬勃发展,但是其长期大量使用也给人类生命健康以及生态环境带来了潜在的生物安全隐患。随着科技与社会进步,饲用抗生素因其种种不可修复的弊端,正逐渐被淘汰,养殖业则正在寻找饲用抗生素替代产品。在这一背景下,“禁抗”与“替抗”概念应运而生。
禁止将饲用抗生素用于动物生产已成为当下全球养殖行业发展的必然趋势。过去几十年,各国先后提出禁抗政策:
1976年,欧盟禁止在饲料中使用四环素类和青霉素类AGP;
1979年,欧盟禁止在饲料中使用竹桃霉素;
1981年,世界卫生组织抗生素慎用联盟成立,呼吁各国政府采取立法手段禁止滥用抗生素AGP;
1986年,瑞典全面禁止在畜禽饲料中使用促生长性抗生素,成为全球首个禁用饲用抗生素的国家;
1995-1997年,丹麦、挪威、德国和欧盟其他成员国陆续禁止使用阿伏霉素;
1998年,丹麦、芬兰分别禁止维吉尼亚霉素和螺旋霉素作为饲料添加剂使用;
1999年,欧盟委员会禁止使用泰乐菌素、螺旋霉素、杆菌肽和维吉尼亚霉素;
2000年,丹麦开始在畜禽饲料中全面禁用促生长类抗生素添加剂,抗生素只限于按处方用于治疗动物疾病;
2002年,欧洲理事会宣布决定逐步淘汰所有促生长用抗生素;
2006年,欧盟成员国全面停止使用其余的所有抗生素生长促进剂;
2011年,韩国宣布了饲料抗生素禁用通知;
2013年,美国FDA发出了自愿禁用指导书;
2014年,美国宣布在未来的三年将逐步禁止AGP的使用;
2016年,世界动物卫生组织(OIE)制定了“同一健康 共同应对抗菌药物耐药行动策略”, 要求各成员履行承诺,按照世界卫生组织-联合国粮农组织-世界动物卫生组织(WHO/FAO/OIE)三方共同制定的“耐药性全球行动计划”要求,参考OIE重要抗菌药物使用标准和指南,制定法规,逐步停止将抗菌药物用作促生长剂;
2017年,美国饲料无AGP处方中停用人类抗生素。
② 国内禁抗的发展历程
在全球共同应对抗菌药物耐药行动策略下,中国农业农村部多次发布公告,分批禁用了数十种原料抗生素。
2015年9月7日,原农业部发布的公告第2292号规定:自2015年12月31日起,停止生产用于食品动物的洛美沙星、培氟沙星、氧氟沙星、诺氟沙星4种原料药的各种盐、酯及其各种制剂;自2016年12月31日起,停止经营、使用用于食品动物的洛美沙星、培氟沙星、氧氟沙星、诺氟沙星4种原料药的各种盐、酯及其各种制剂。
2016年7月26日,原农业部发布的公告第2428号规定:停止硫酸黏菌素用于动物促生长。
2017年10月20日,原农业部发布的公告第2583号规定:禁止非泼罗尼及相关制剂用于食品动物。
2018年2月20日,原农业部发布的公告第2638号规定:自2018年5月1日起,停止生产喹乙醇、氨苯胂酸、洛克沙胂等3种兽药的原料药及各种制剂,相关企业的兽药产品批准文号同时注销;2019年5月1日起,停止经营、使用喹乙醇、氨苯胂酸、洛克沙胂等3种兽药的原料药及各种制剂。
2019年7月9日,农业农村部发布了公告第194号规定:自2020年1月1日起,退出除中药外的所有促生长类药物饲料添加剂品种。
这也标志我国进入“全面禁抗”时代。
③ 潜在替抗方案
随着全球饲用禁抗进程深入,寻找安全有效的饲用抗生素替代品成为全球研究的热点,市场迫切需求安全、高效的饲用抗生素替代产品。饲料行业已开始寻求和开发绿色、无污染、低残留的饲料添加剂和技术方案以替代抗生素的使用。
1. 益生菌
益生菌制剂作为当前畜牧业养殖中替代饲用抗生素的新型饲料添加剂(表1),在饲用效果、饲喂安全性等方面均有显著优势,目前已广泛应用到畜禽养殖生产实践中。其中乳酸菌类益生菌由于耐受性能优异,被众多学者认为是最有前途的饲用抗生素替代品。
益生菌的优势包括可以抑制有害菌生长繁殖,增强非特性免疫功能,利于机体良性发展,有助于预防疾病等。缺点是:适用于治未病,疾病爆发时,达不到抗生素的使用效果;菌群平衡点难以控制,构建周期长,影响因素多,难以追踪效果;微生物在生产、运输和储存中易失活,不稳定。
2. 益生元
益生元是一类不易被消化的物质,目前大多数商业用益生元为寡糖,如菊粉、低聚木糖、低聚果糖、低聚异麦糖、抗性淀粉等。
益生元的优势是其可以选择性地促进动物肠道中双歧杆菌、乳酸杆菌等有益微生物生长,从而对宿主产生多种有益影响,如促进生长和增重。但是由于益生元本身无杀菌作用,所以只能辅助抗病和防病,并且其促生长作用表现不一。
3. 噬菌体
噬菌体是一种可以感染细菌的病毒。噬菌体的优势是其具有高度特异性,这意味着噬菌体对动物体的副作用小。此外,噬菌体的靶向性很强,每一种噬菌体只攻击一种类型的细菌,因此噬菌体治疗不会损伤机体内无害的细菌。但是其缺点是噬菌体只能杀死其所靶向的细菌,而且主要是外用,若有体内感染,或者全身感染,则往往不能到达发病部位。
4. 饲用酶制剂
根据饲用酶制剂的功能作用,分为:具有直接营养功能的淀粉酶、蛋白酶、脂肪酶;降低日粮黏性,减少有害微生物繁殖的木聚糖酶、葡聚糖酶、纤维素酶;降低日粮免疫原性,减少肠道病变坏死的蛋白酶、甘露聚糖酶、半乳糖酶;直接杀灭细菌,抑制病原菌危害的葡萄糖氧化酶、溶菌酶、果胶酶。
酶制剂的优势是种类多样,可以通过多种途径来促进生长,如:补充内源酶促进消化;特异性地降低饲料中抗营养因子水平来实现提高饲料转化率;调节肠道微生态,抑制病原菌生长。
但存在的问题是:(1)不同条件下的酶活差异较大;(2)作用效果受酶种类、动物品种、年龄及健康状况等多种因素影响;(3)不同种类酶制剂的配合使用工作较繁琐,难摸清。
5. 酸化剂
市售产品主要是复合酸化剂,由无机酸和有机酸组成,其中无机酸包括磷酸和盐酸,有机酸包括柠檬酸、延胡索酸、苹果酸、山梨酸、琥珀酸、乳酸、富马酸、甲酸、乙酸、丙酸和丁酸等。
酸化剂的促生长方式包括:(1)可以降低胃肠道的pH值,起到对大肠杆菌、沙门氏菌、葡萄球菌和梭菌的杀菌、抑菌作用;(2)促进生长和消化吸收,调节肠道菌群结构和平衡;(3)参与物质合成与代谢,促进矿物质等营养物质的吸收。该类产品的稳定性高,储存运输对其影响较小。
缺点是:(1)剂量与范围有待确定,不同剂量的作用效果差别较大;(2)刺激性和挥发性限制了酸化剂在动物生产中的应用;(3)对设备、料槽等造成腐蚀等。
6. 抗菌肽
抗菌肽又称抗微生物肽或宿主防御肽,是生物体经诱导产生的具有广谱抗菌活性和免疫调节活性的一类活性多肽,属于机体非特异性防御系统的固有组成部分。
抗菌肽的优势包括:(1)直接作用于细菌、真菌等,抑制其生长繁殖;(2)热稳定性好,能够耐受饲料加工过程中高温高压的剧烈条件。
缺点包括:(1)毒理性方面的研究还不够深入;(2)生产工艺多为生物提取,生产成本及应用成本高;(3)抗菌肽抗菌谱一般较窄,只能用来应对特定范围内的病原菌。
7. 中草药
目前在养殖业上使用较多的中草药种类有白头翁、黄芪、黄连、党参、大黄、炙甘草等。
中草药的优势是来源广泛、价格低廉、安全方便、毒副作用小、无残留、无抗药性。
缺点是:(1)中草药药效成分复杂而且易受原料产地和采收季节等因素的影响,使其药效和质量不稳定,所以应用效果常不一致;(2)大部分中草药都作用较慢,所需剂量较大;(3)有效添加剂量过高(5%-20%),使其应用成本较高;(4)缺乏有关其饲用安全性的科学数据。
8. 植物提取物
植物提取物的有效成分主要有皂苷、生物碱、多糖、糖萜素、茶多酚、黄酮、精油等。
优势是具有抑菌、抗病毒、抗氧化等作用,且毒副作用小、无抗药性。
缺点是:(1)质量不稳定,植物品种、种植地、收获时间、使用部位等不同会导致其活性成分差异大;(2)产品标准不统一;(3)研究方向单一,实际应用效果不确定;(4)加工工艺落后,利用效率低。
作者:热心肠小伙伴们
来源:《2023肠道产业发展白皮书》
编辑:豫小鱼
临床研究诊断试剂
2023-02-15
今日,BioBAY园内上市企业信达生物宣布其研发的重组抗胰岛素样生长因子1受体(IGF-1R)抗体注射液(研发代号:IBI311)在甲状腺相关眼病(TAO)受试者的2期临床研究中完成首例受试者给药。该项研究是一项在TAO受试者中开展的随机、双盲、安慰剂对照的2期临床研究。主要目的是评估IBI311改善TAO受试者突眼的疗效,以支持IBI311的关键注册临床开发。IBI311是信达生物制药研发的靶向IGF-1R的单克隆抗体,用于治疗甲状腺相关性眼病等疾病。IBI311可通过阻断IGF-1与IGF-1R结合,抑制IGF-1R介导的信号通路激活,减少下游炎症因子的表达,从而抑制眼眶成纤维细胞(OFs)的活化及其活化导致的透明质酸和其他糖胺聚糖的合成,减轻眼外肌和眼眶软组织的炎症反应;抑制OFs分化为脂肪细胞或肌成纤维细胞,进而减轻TAO患者的疾病活动度,改善突眼、复视、眼部充血水肿等症状。目前,替妥木单抗(Teprotumumab)是海外唯一获FDA批准的用于TAO治疗的药物,国内尚未有针对TAO的药物获批。TAO是一种累及眼部组织的自身免疫性疾病,通常伴发于毒性弥漫性甲状腺肿(Graves病,GD),又称甲状腺相关眼病(Thyroid eye disease, TED),是成人中最常见的眼眶相关疾病。目前,TAO的发病机制尚不完全清楚,但多项研究表明,存在于肌纤维、眼眶纤维结缔组织间隙中的OFs是导致TAO眼眶软组织增生的关键因素。TAO通常为轻度到中重度,约3~5%的TAO患者会发展至极重度,表现为威胁视力的角膜溃疡或压迫性视神经病变等。除了可能影响外观和视功能,TAO对患者的社交功能和生活质量产生极其严重的影响。该临床研究的主要研究者、中国工程院院士、上海交通大学医学院附属第九人民医院眼科范先群教授表示:“甲状腺相关眼病是成年人最常见的眼眶病之一,是与甲状腺疾病密切相关的一种器官特异性自身免疫性疾病,可严重影响患者的视功能和外观。当前国内尚无靶向药物获批用于治疗甲状腺相关眼病。2020年,替妥木单抗被FDA批准用于治疗TAO,为TAO治疗提供了新的选择,并被中国甲状腺相关眼病临床诊断和治疗指南(2022年)、欧洲Graves眼眶病协作组(EUGOGO)和美国甲状腺学会和欧洲甲状腺学会的甲状腺眼病共识推荐。我们非常期待由国内创新药企业开发的IBI311能在中国甲状腺相关眼病人群中展现出良好的有效性和安全性,并尽快上市,减轻患者病痛。”信达生物制药集团临床开发副总裁钱镭博士表示:“当前中国尚无靶向药物获批用于治疗甲状腺相关眼病,该领域有着极大的未满足的临床需求。IBI311是信达生物研发的用于治疗TAO的重组抗IGF-1R抗体,也是我们在眼科领域布局的又一新靶点分子,具有较高的成药性。体外及临床前动物研究已经初步验证了IBI311具有良好的安全性及生物学活性;在健康人群中开展的的I期临床研究同样提示IBI311具有良好的安全性及耐受性,为进一步的临床开发提供依据。我有信心IBI311在TAO受试者中开展的II期临床研究也会看到积极的疗效和一致的安全性。信达将与学术界通力合作,在范院士引领下全力推动IBI311的临床开发,把高质量、高可及性的生物药带给中国TAO患者,真正实践‘开发出老百姓用得起的高质量生物药’的信达使命。”▌文章来源:信达生物责编:何文正校对:杜姝审核:任旭推荐阅读上市企业丨和铂医药:超6亿美元!B7H4x4-1BB双抗成功“出海”上市企业丨开拓药业:积极顶线!全球首个外用PROTAC药物美国1期临床数据公布上市企业丨和铂医药:CCR8单抗在美国获批临床,一个月内三获IND批件
临床2期临床1期
2023-02-15
·信达生物
2023年02月15日,美国罗克维尔和中国苏州——信达生物制药集团(香港联交所股票代码:01801),一家致力于研发、生产和销售肿瘤、自免、代谢、眼科等重大疾病领域创新药物的生物制药公司,宣布其研发的重组抗胰岛素样生长因子1受体(IGF-1R)抗体注射液(研发代号:IBI311)在甲状腺相关眼病(thyroid associated ophthalmopathy, TAO)受试者的II期临床研究中完成首例受试者给药。该项研究(CTR20223393)是一项在TAO受试者中开展的随机、双盲、安慰剂对照的II期临床研究。主要目的是评估IBI311改善TAO受试者突眼的疗效,以支持IBI311的关键注册临床开发。IBI311是信达生物制药研发的靶向IGF-1R的单克隆抗体,用于治疗甲状腺相关性眼病等疾病。IBI311可通过阻断IGF-1与 IGF-1R结合,抑制IGF-1R介导的信号通路激活,减少下游炎症因子的表达,从而抑制眼眶成纤维细胞(OFs)的活化及其活化导致的透明质酸和其他糖胺聚糖的合成,减轻眼外肌和眼眶软组织的炎症反应;抑制OFs分化为脂肪细胞或肌成纤维细胞,进而减轻TAO患者的疾病活动度,改善突眼、复视、眼部充血水肿等症状。目前,替妥木单抗(Teprotumumab)是海外唯一获FDA批准的用于TAO治疗的药物,国内尚未有针对TAO的药物获批。该临床研究的主要研究者、中国工程院院士、上海交通大学医学院附属第九人民医院眼科范先群教授表示:“甲状腺相关眼病是成年人最常见的眼眶病之一,是与甲状腺疾病密切相关的一种器官特异性自身免疫性疾病,可严重影响患者的视功能和外观。当前国内尚无靶向药物获批用于治疗甲状腺相关眼病。2020年,替妥木单抗被FDA批准用于治疗TAO,为TAO治疗提供了新的选择,并被中国甲状腺相关眼病临床诊断和治疗指南(2022年)、欧洲Graves 眼眶病协作组(EUGOGO)和美国甲状腺学会和欧洲甲状腺学会的甲状腺眼病共识推荐。我们非常期待由国内创新药企业开发的IBI311能在中国甲状腺相关眼病人群中展现出良好的有效性和安全性,并尽快上市,减轻患者病痛。”信达生物制药集团临床开发副总裁钱镭博士表示:“当前中国尚无靶向药物获批用于治疗甲状腺相关眼病,该领域有着极大的未满足的临床需求。IBI311是信达生物研发的用于治疗TAO的重组抗IGF-1R抗体,也是我们在眼科领域布局的又一新靶点分子,具有较高的成药性。体外及临床前动物研究已经初步验证了IBI311具有良好的安全性及生物学活性;在健康人群中开展的的I期临床研究同样提示IBI311具有良好的安全性及耐受性,为进一步的临床开发提供依据。我有信心IBI311在TAO受试者中开展的II期临床研究也会看到积极的疗效和一致的安全性。信达将与学术界通力合作,在范院士引领下全力推动IBI311的临床开发,把高质量、高可及性的生物药带给中国TAO患者,真正实践‘开发出老百姓用得起的高质量生物药’的信达使命。”关于甲状腺相关眼病(TAO)- 滑动查看更多介绍 -TAO是一种累及眼部组织的自身免疫性疾病,通常伴发于毒性弥漫性甲状腺肿(Graves病,GD),又称甲状腺相关眼病(Thyroid eye disease, TED),是成人中最常见的眼眶相关疾病。TAO可见于大约25~50%的GD患者,也可见于其他甲状腺疾病,甚至甲状腺功能正常者1。TAO的年发病率预估为16/100,000人(女性)和2.9/100,000人(男性)2。按照疾病严重程度,可分为轻度、中重度和极重度。虽然TAO更常发生于女性,但重度病例更常发生于男性。TAO最常见于30~50岁的患者,严重TAO病例更常发生于50岁以上的患者3。目前,TAO的发病机制尚不完全清楚,但多项研究表明,存在于肌纤维、眼眶纤维结缔组织间隙中的OFs是导致TAO眼眶软组织增生的关键因素4。TAO的自然病程分为活动期和非活动期5。最常见的症状是眼干、眼部异物感、畏光、流泪、复视和眼后压迫感,而典型的体征包括眼球突出、上眼睑退缩、眼睑水肿、眶周组织和球结膜水肿。TAO通常为轻度到中重度,约3~5%的TAO患者会发展至极重度,表现为威胁视力的角膜溃疡或压迫性视神经病变等6。除了可能影响外观和视功能,TAO对患者的社交功能和生活质量产生极其严重的影响。目前,中重度活动性TAO的一线治疗方案为糖皮质激素静脉冲击治疗,存在突眼改善不理想以及激素相关的全身副作用等问题,仍存在较大的未满足的临床需求。二线治疗包括再次激素冲击或联合眼眶放疗或其他免疫调节剂。2020年获得FDA批准上市的替妥木单抗(Teprotumumab)也被EUGOGO 指南7和中国甲状腺相关眼病临床诊断和治疗指南(2022年)8和美国甲状腺学会和欧洲甲状腺学会的甲状腺眼病共识9推荐为中重度活动性TAO的二线治疗方案。关于IBI311- 滑动查看更多介绍 -IBI311是信达生物制药研发的重组抗胰岛素样生长因子1受体(IGF-1R)抗体,用于治疗TAO。IGF-1R是一种跨膜酪氨酸激酶受体,在发育、代谢及免疫调节中发挥作用,并在TAO患者的OFs、B细胞、T细胞中过表达10。IBI311可阻断IGF-1等相关配体或激动型抗体介导的 IGF-1R 信号通路激活,减少下游炎症因子的表达,从而抑制OFs 活化导致的透明质酸和其他糖胺聚糖合成,减轻炎症反应;抑制OFs 分化为脂肪细胞或肌成纤维细胞,进而减轻TAO患者的疾病活动度,改善突眼、复视、眼部充血水肿等症状和体征。关于信达生物- 滑动查看更多介绍 -“始于信,达于行”,开发出老百姓用得起的高质量生物药,是信达生物的理想和目标。信达生物成立于2011年,致力于开发、生产和销售肿瘤、代谢、自身免疫、眼科等重大疾病领域的创新药物。2018年10月31日,信达生物制药在香港联合交易所有限公司主板上市,股票代码:01801。自成立以来,公司凭借创新成果和国际化的运营模式在众多生物制药公司中脱颖而出。建立起了一条包括36个新药品种的产品链,覆盖肿瘤、自身免疫、代谢、眼科等多个疾病领域,其中7个品种入选国家“重大新药创制”专项。公司已有8个产品(信迪利单抗注射液,商品名:达伯舒®,英文商标:TYVYT®;贝伐珠单抗生物类似药,商品名:达攸同®,英文商标:BYVASDA ®;阿达木单抗生物类似药,商品名:苏立信®,英文商标:SULINNO ®;利妥昔单抗生物类似药,商品名:达伯华®,英文商标:HALPRYZA®;佩米替尼片,商品名:达伯坦®,英文商标:PEMAZYRE®;奥雷巴替尼片,商品名:耐立克®;雷莫西尤单抗,商品名:希冉择®,英文商标:CYRAMZA®;塞普替尼,商品名:睿妥®,英文商标:Retsevmo®)获得批准上市,3个品种在NMPA审评中,6个新药分子进入III期或关键性临床研究,另外还有19个新药品种已进入临床研究。信达生物已组建了一支具有国际先进水平的高端生物药开发、产业化人才团队,包括众多海归专家,并与美国礼来制药、赛诺菲、Adimab、Incyte、MD Anderson 癌症中心等国际合作方达成战略合作。信达生物希望和大家一起努力,提高中国生物制药产业的发展水平,以满足百姓用药可及性和人民对生命健康美好愿望的追求。详情请访问公司网站:www.innoventbio.com或公司领英账号:Innovent Biologics。声明:1. 该适应症为研究中的药品用法,尚未在中国获批;2. 信达不推荐任何未获批的药品/适应症使用。参考文献:1.Li Z, Cestari D M, Fortin E. Thyroid eye disease: what is new to know? Curr Opin Ophthalmol. 2018;29(6):528-534.2.Bartley G. The epidemiological characteristics and clinical course of ophthalmology associated with autoimmune thyroid disease in Olmsted Country, Minnesota. Trans Am Ophthalmol Soc 1994;92:477-588.3.Edsel I. Thyroid Associated Orbitopathy. Retrieved June 7, 2011, from Medscape Reference: http://emedicine.medscape.com/article/1218444-overview#a14.Ali F, Chorsiya A, Anjum V, Ali A. Teprotumumab (TEPEZZA): from the discovery and development of medicines to USFDA approval for active thyroid eye disease (TED) treatment. Int Ophthalmol. 2021;41(4):1549-1561. 5.Dolman P J. Evaluating Graves’ orbitopathy. Best Pract Res Clin Endocrinol Metab.2012;26(3):229-248.6.Bahn R S. Graves’ ophthalmopathy. N Engl J Med. 2010;362(8):726-738.7.Bartalena L, Kahaly GJ, Baldeschi L, et al. The 2021 European Group on Graves’ orbitopathy (EUGOGO) clinical practice guidelines for the medical management of Graves’ orbitopathy. Eur J Endocrinol. 2021;185(4):G43-G67.8.中华医学会眼科学分会眼整形眼眶病学组, 中华医学会内分泌学分会甲状腺学组. 中国甲状腺相关眼病诊断和治疗指南 (2022年).中华眼科杂志. 2022;58(9).9.Burch HB, et al. Management of thyroid eye disease: a Consensus Statement by the American Thyroid Association and the European Thyroid Association. Eur Thyroid J. 2022;11(6):e220189.10.Douglas RS, Naik V, Hwang CJ, et al. B cells from patients with Graves’ disease aberrantly express the IGF-1 receptor: implications for disease pathogenesis. J Immunol 2008;181:5768-5774.信达生物前瞻性声明本新闻稿所发布的信息中可能会包含某些前瞻性表述。这些表述本质上具有相当风险和不确定性。在使用“预期”、“相信”、“预测”、“期望”、“打算”及其他类似词语进行表述时,凡与本公司有关的,目的均是要指明其属前瞻性表述。本公司并无义务不断地更新这些预测性陈述。这些前瞻性表述乃基于本公司管理层在做出表述时对未来事务的现有看法、假设、期望、估计、预测和理解。这些表述并非对未来发展的保证,会受到风险、不确性及其他因素的影响,有些乃超出本公司的控制范围,难以预计。因此,受我们的业务、竞争环境、政治、经济、法律和社会情况的未来变化及发展的影响,实际结果可能会与前瞻性表述所含资料有较大差别。本公司、本公司董事及雇员代理概不承担 (a) 更正或更新本网站所载前瞻性表述的任何义务;及 (b) 若因任何前瞻性表述不能实现或变成不正确而引致的任何责任。
临床1期临床2期
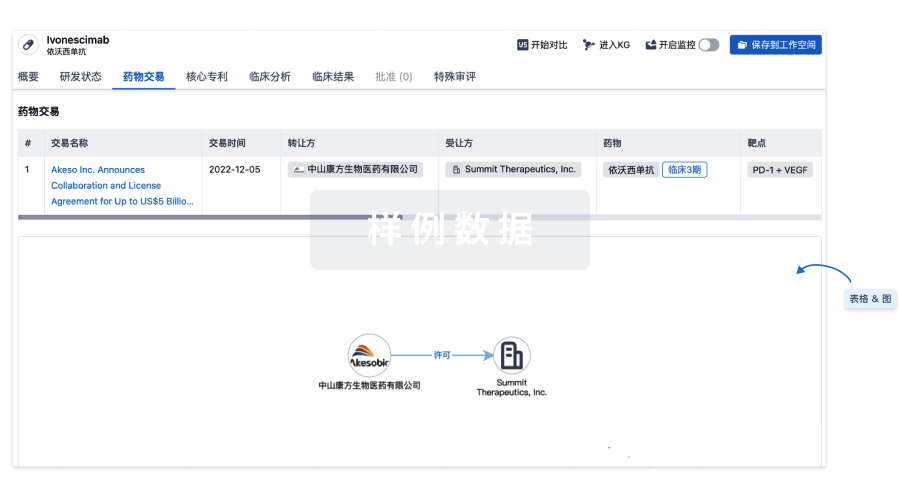
100 项与 醋竹桃霉素 相关的药物交易
登录后查看更多信息
研发状态
10 条最早获批的记录, 后查看更多信息
登录
| 适应症 | 国家/地区 | 公司 | 日期 |
|---|---|---|---|
| 细菌感染 | 美国 | 1969-05-27 |
登录后查看更多信息
临床结果
临床结果
适应症
分期
评价
查看全部结果
| 研究 | 分期 | 人群特征 | 评价人数 | 分组 | 结果 | 评价 | 发布日期 |
|---|
No Data | |||||||
登录后查看更多信息
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
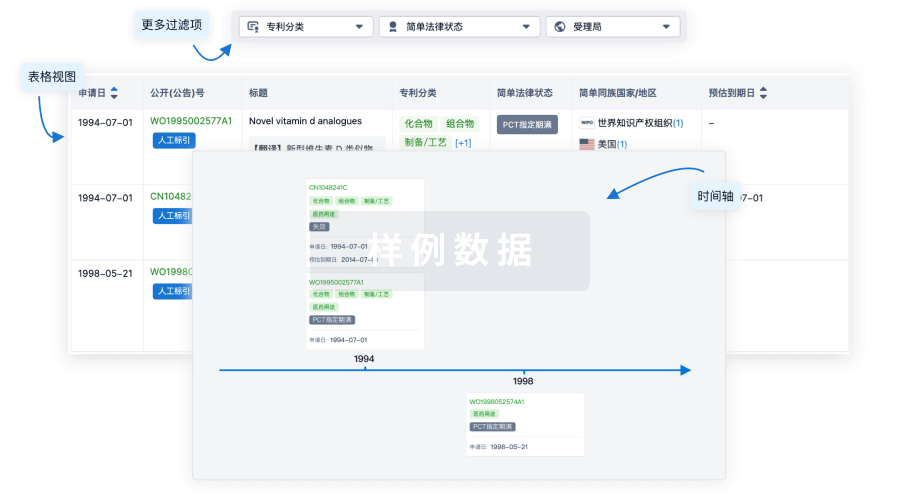
核心专利
使用我们的核心专利数据促进您的研究。
登录
或
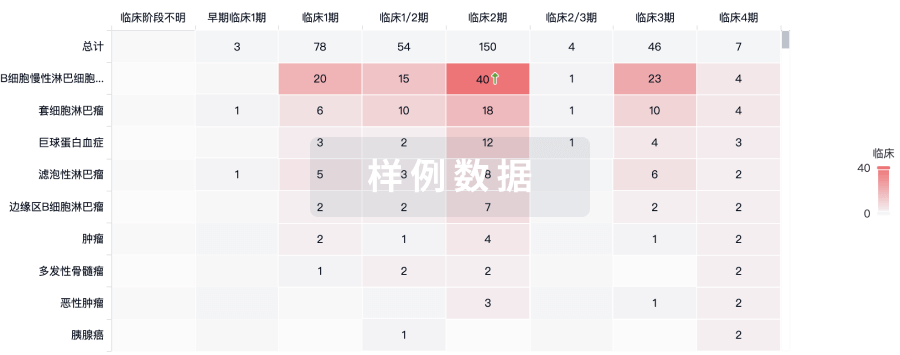
临床分析
紧跟全球注册中心的最新临床试验。
登录
或
批准
利用最新的监管批准信息加速您的研究。
登录
或

特殊审评
只需点击几下即可了解关键药物信息。
登录
或

Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用