预约演示
更新于:2025-07-31
Recombinant canarypox virus-based vaccine(Therion Biologics Corp.)
更新于:2025-07-31
概要
基本信息
在研机构- |
权益机构- |
最高研发阶段终止临床2期 |
首次获批日期- |
最高研发阶段(中国)- |
特殊审评- |
登录后查看时间轴
关联
4
项与 Recombinant canarypox virus-based vaccine(Therion Biologics Corp.) 相关的临床试验ChiCTR2300072012
Prospective single-arm clinical study of TBC as conditioning regimen for haplo-identical hematopoietic stem cell transplantation in refractory / relapsed acute myeloid leukemia
开始日期2022-11-08 |
申办/合作机构- |
NCT03050814
A Randomized Phase II Trial of Standard of Care Alone or in Combination With Ad-CEA Vaccine and Avelumab in Patients With Previously Untreated Metastatic or Unresectable Colorectal Cancer
Background:
Colorectal cancer is a common cancer in the Unites States (U.S.) It causes the second most cancer-related deaths. The drug avelumab and vaccine Ad-CEA together help the immune system fight cancer.
Objective:
To test if avelumab and Ad-CEA plus standard therapy treats colorectal cancer that has spread to other sites better than standard therapy alone.
Eligibility:
People ages 18 and older with untreated colorectal cancer that has spread in the body
Design:
Participants will be screened with:
Test to see if their cancer has a certain deficiency
Blood, urine, and heart tests
Scans
Medical history
Physical exam
Tumor sample. This can be from a previous procedure.
A small group of participants will get Ad-CEA and avelumab plus standard therapy. This is leucovorin calcium (folinic acid), fluorouracil, and oxaliplatin (FOLFOX) plus bevacizumab for up to 24 weeks then capecitabine plus bevacizumab.
The others will have treatment in 2-week cycles. They will be Arm A or B:
Arm A: FOLFOX and bevacizumab by intravenous (IV) days 1 and 2 for 12 cycles. After that, capecitabine by mouth twice a day and bevacizumab by IV on day 1.
Arm B: Ad-CEA injection every 2-12 weeks. Avelumab by IV on day 1 of each cycle. FOLFOX and bevacizumab by IV days 2 and 3 for 12 cycles. Then, capecitabine by mouth twice a day and bevacizumab through IV on day 2.
Participants will repeat screening tests during the study.
Participants will be treated until their disease gets worse or they have bad side effects. Arm A participants can join Arm B. They will have a visit 4 5 weeks after they stop therapy.
Colorectal cancer is a common cancer in the Unites States (U.S.) It causes the second most cancer-related deaths. The drug avelumab and vaccine Ad-CEA together help the immune system fight cancer.
Objective:
To test if avelumab and Ad-CEA plus standard therapy treats colorectal cancer that has spread to other sites better than standard therapy alone.
Eligibility:
People ages 18 and older with untreated colorectal cancer that has spread in the body
Design:
Participants will be screened with:
Test to see if their cancer has a certain deficiency
Blood, urine, and heart tests
Scans
Medical history
Physical exam
Tumor sample. This can be from a previous procedure.
A small group of participants will get Ad-CEA and avelumab plus standard therapy. This is leucovorin calcium (folinic acid), fluorouracil, and oxaliplatin (FOLFOX) plus bevacizumab for up to 24 weeks then capecitabine plus bevacizumab.
The others will have treatment in 2-week cycles. They will be Arm A or B:
Arm A: FOLFOX and bevacizumab by intravenous (IV) days 1 and 2 for 12 cycles. After that, capecitabine by mouth twice a day and bevacizumab by IV on day 1.
Arm B: Ad-CEA injection every 2-12 weeks. Avelumab by IV on day 1 of each cycle. FOLFOX and bevacizumab by IV days 2 and 3 for 12 cycles. Then, capecitabine by mouth twice a day and bevacizumab through IV on day 2.
Participants will repeat screening tests during the study.
Participants will be treated until their disease gets worse or they have bad side effects. Arm A participants can join Arm B. They will have a visit 4 5 weeks after they stop therapy.
开始日期2017-04-05 |
申办/合作机构 |
NCT00027833
Pilot Phase II Study of Safety and Immunogenicity of an ALVAC-CEA/B7.1 Vaccine Administered With Chemotherapy, Alone or in Combination With Tetanus Toxoid, as Compared to Chemotherapy Alone, in Patients With Metastatic Colorectal Adenocarcinoma
RATIONALE: Vaccines may make the body build an immune response to kill tumor cells. Drugs used in chemotherapy use different ways to stop tumor cells from dividing so they stop growing or die. Tetanus toxoid may make tumor cells more sensitive to chemotherapy and vaccine therapy.
PURPOSE: Randomized phase II trial to study the effectiveness of chemotherapy and vaccine therapy with or without tetanus toxoid compared with chemotherapy alone in treating patients who have metastatic colorectal cancer.
PURPOSE: Randomized phase II trial to study the effectiveness of chemotherapy and vaccine therapy with or without tetanus toxoid compared with chemotherapy alone in treating patients who have metastatic colorectal cancer.
开始日期2001-12-01 |
申办/合作机构 |
100 项与 Recombinant canarypox virus-based vaccine(Therion Biologics Corp.) 相关的临床结果
登录后查看更多信息
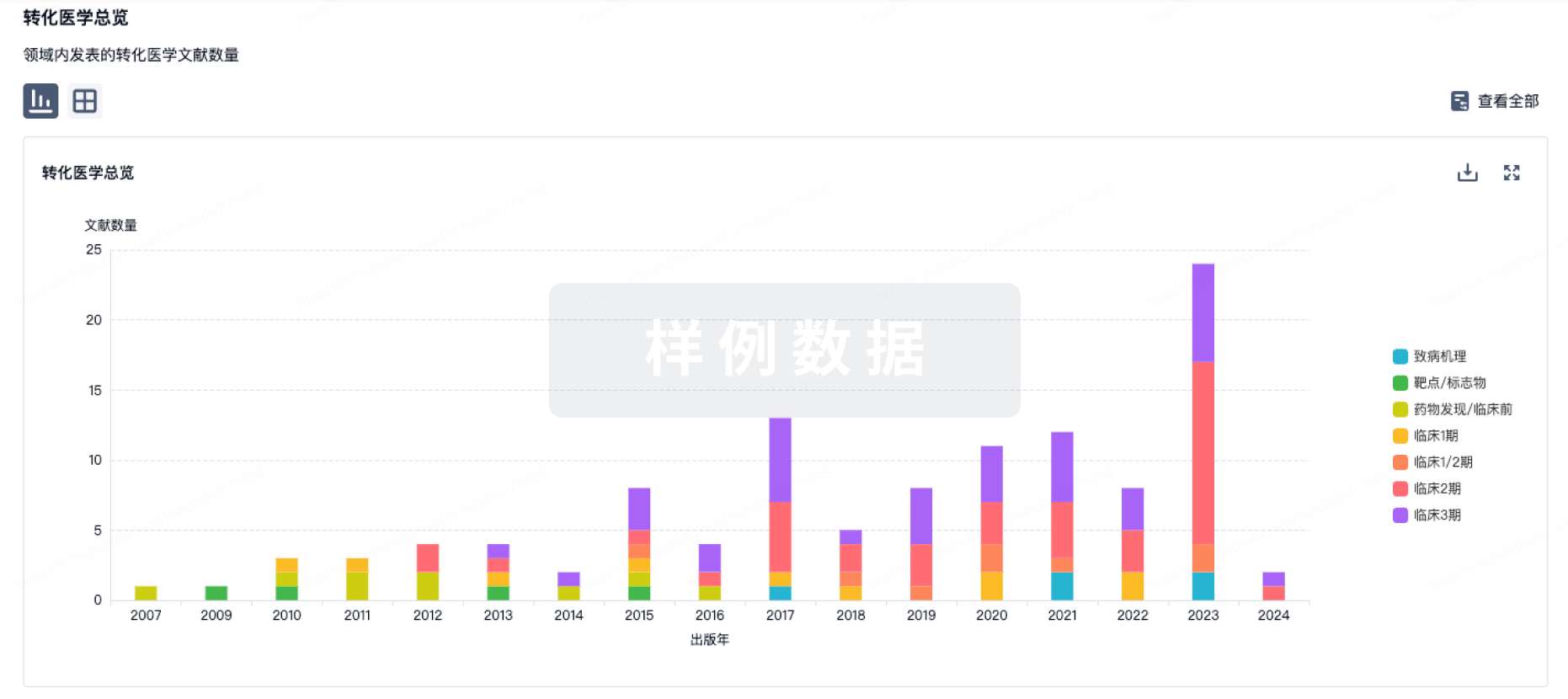
100 项与 Recombinant canarypox virus-based vaccine(Therion Biologics Corp.) 相关的转化医学
登录后查看更多信息
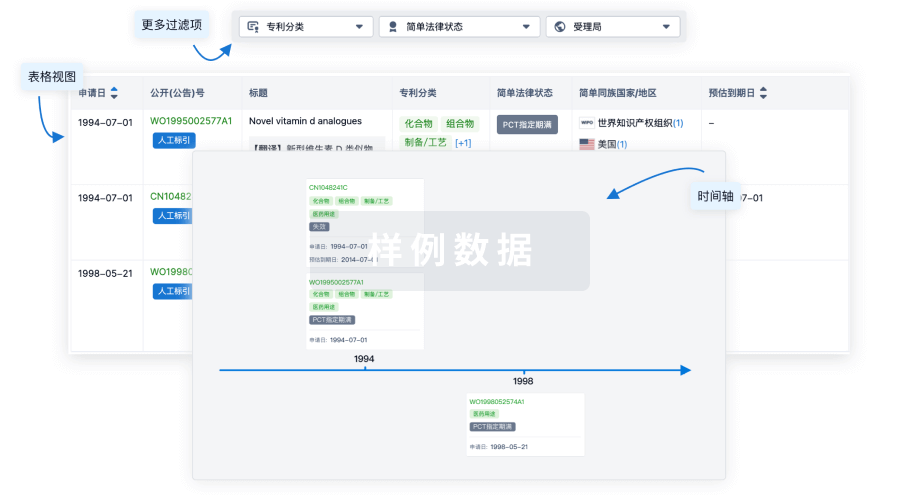
100 项与 Recombinant canarypox virus-based vaccine(Therion Biologics Corp.) 相关的专利(医药)
登录后查看更多信息
261
项与 Recombinant canarypox virus-based vaccine(Therion Biologics Corp.) 相关的文献(医药)2025-06-15·PHYTOMEDICINE
Integration of heart-on-a-chip and metabolomics for understanding the toxicity-attenuating effect of ethnomedicinal processing.
Article
作者: Liu, Yue ; Cui, Mengyang ; Liang, Qionglin ; Xu, Xinmei ; Cheung, Suet ; Yu, Shufu ; Zhang, Yi ; Ai, Yongjian
BACKGROUND:
Tiebangchui (TBC), is a well-known traditional Tibetan medicine that coexists with toxicity and effects. Highland barley wine is an effective and unique processing method to reduce TBC's toxic side effects. However, the toxicity reduction mechanism is ambiguous and needs to be explored urgently. Meanwhile, the limitations of traditional animal models and two-dimensional (2D) cell culture models urgently require the development of more reliable analytical platforms for drug detection.
STUDY DESIGN:
The integrated metabolomics and biomimetic 3D anisotropic heart-on-a-chip were utilized to reveal the toxicity-attenuating effect of highland barley wine-processed TBC from the dual perspectives of in vitro compositional changes and in vivo toxicity mechanisms. The combination of organ-on-a-chip and metabolomics provides a powerful tool for achieving spatiotemporal control of cell growth and biochemistry, as well as rapid detection of small molecule metabolites.
METHODS:
Ultra-performance liquid chromatography-quadrupole time-of-flight mass spectrometry (UPLC-Q-TOF-MS) coupled with global natural products social molecular networking (GNPS) was utilized for the expeditious identification of chemical constituents in both raw and processed TBC products. Multivariate statistical analysis was applied to screen for differential constituents before and after processing, followed by quantification of these constituents using ultra-performance liquid chromatography-triple quadrupole tandem mass spectrometry (UPLC-QqQ-MS/MS). After constructing a 3D heart-on-a-chip model, the structure and function of the chip model were validated via COMSOL finite element analysis, immunofluorescence, and qPCR. Leveraging this chip model, integrating molecular biology and metabolomics was employed to further elucidate the detoxification mechanism by highland barley wine-processed TBC.
RESULTS:
The comprehensive analytical strategies demonstrated that the loss of the toxic constituents of TBC through leaching during steeping and the esterification of diterpene alkaloids with long-chain fatty acids in highland barley wine to produce less toxic lipid alkaloids were the main mechanisms of toxicity reduction. Furthermore, a biomimetic 3D anisotropic heart-on-a-chip was fabricated to evaluate differences in cardiotoxicity before and after processing. The results illustrated that the raw TBC and aconitine caused a significant increase in the extracellular LDH level, resulting in intracellular Ca2+ overload, substantial ROS production, and metabolite disorders primarily associated with the tricarboxylic acid cycle. This cascade of reactions ultimately led to apoptosis; however, highland barley wine processing of TBC mitigated these cardiotoxic effects.
CONCLUSION:
This work not only revealed the toxicity-reducing mechanism of highland barley wine-processed TBC but also provided a novel paradigm for drug toxicity evaluation integrating metabolomics and organ-on-a-chip technologies.
2025-05-20·ANALYTICAL CHEMISTRY
Biomimetic Microparticles with Myocardial and Endocardial Integration for Drug Toxicity Studies
Article
作者: Zhang, Yingrui ; Meng, Xian-Li ; Chen, Shiyu ; Wu, Zengnan ; Zhang, Yi ; Xu, Tong ; Lin, Jin-Ming
Hydrogel microparticles are versatile tools for organ modeling due to their simplicity, uniformity, and customizability, yet their limited physiological relevance constrains practical applications. In this study, a heart microparticle model that incorporates endocardial and myocardial structures and functions was developed. Hydrogel microparticles with rough surfaces, embedded with cardiomyocytes, were created using a custom-designed microfluidic device. Surface modification with matrigel enhanced the adhesion and connectivity of endothelial cells, enabling the formation of a densely packed endothelial layer. Real-time analysis, combining microparticle culture with a microfluidic chip-mass spectrometry system, demonstrated the utility of these particles in detecting the cardiotoxicity of heart-related drugs. For example, the analysis revealed that the cardiotoxicity of aconitine and Tie-bang-chui (TBC) was associated with elevated lactate and succinate levels, while processed TBC mitigated this toxicity of TBC by reducing these metabolites. These biomimetic microparticle models provide a novel platform for real-time metabolite analysis and cardiotoxicity research.
2025-05-07·ACS Applied Materials & Interfaces
In Situ Synthesis of Plasticized Bacterial Cellulose Films for Daily Packaging Using Biobased Plasticizers
Article
作者: Zhang, Haibo ; Dai, Wenxue ; Deng, Shuaijun ; Chen, Guoqiang ; Zhang, Yibing ; Yan, Yihai ; Afreen, Shagufta ; Wang, Lei
Bacterial cellulose (BC) naturally decomposes in the environment without releasing toxins or microplastics, making it a promising alternative to conventional plastics. However, its inherent brittleness after drying limits its broader application. This study investigates four biobased plasticizers─epoxy soybean oil, castor oil, tributyl citrate (TBC), and tributyl trans-aconitate (TBA)─to enhance the flexibility of BC through in situ modification. By combining a gel-assisted biosynthesis with an in situ spray plasticization method, biobased plasticizers are uniformly incorporated into the nanofiber network of BC, resulting in films with significantly improved flexibility and transparency. Among the biobased plasticizers, TBC and TBA showed the most effective plasticization, increasing the E% to 9.63 and 11.90%, respectively, corresponding to 6.3-fold and 7.5-fold enhancements compared to the control. This approach not only improves the mechanical properties of BC but also streamlines production by enabling a simplified processing method. The findings underscore the potential of plasticized BC biomaterials in replacing fossil-based plastics and advancing the development of sustainable materials.
1
项与 Recombinant canarypox virus-based vaccine(Therion Biologics Corp.) 相关的新闻(医药)2025-06-02
·医药速览
Summary免疫系统具有区分自身和非自身的能力,即所谓的免疫耐受或“免疫系统的意识”,这种意识旨在通过消除表达一系列非自身抗原(包括微生物衍生肽段)的细胞来实现宿主保护。这种成功的免疫反应伴随着一系列可溶性介质的分泌,例如细胞因子和趋化因子,它们不仅有助于清除受感染的宿主细胞,还能激活不针对原始特异性抗原的T细胞,这种非特异性的T细胞激活被称为“旁观者激活(bystander activation)”。虽然已明确这一现象依赖于细胞因子,但文献证据显示,根据T细胞亚群(初始T细胞与记忆T细胞)的不同,自身肽/MHC复合体的识别也参与其中。在本文中,我们将总结当前对旁观者T细胞激活机制的理解,以及其在多种疾病(包括微生物感染、癌症、自身免疫和同种异体免疫以及动脉粥样硬化等慢性炎症疾病)中的生物学意义。01引言牛津语言词典将“旁观者(bystander)”定义为在正在进行的特定事件中在场但未直接参与的人。自然界中充满了可能具有共生益处或有害后果的旁观者例子,例如在光合作用过程中,绿叶植物会释放氧气作为副产品。因此,真核生物可以利用释放的氧气进行细胞呼吸,产生细胞能量。这一相互关联的事件链清楚地展示了旁观者效应,其中真核细胞不一定直接参与光合作用,但可以通过使用氧气副产品而受益。细胞因子作为功能免疫反应的副产物,可以激活包括T细胞在内的多种免疫细胞,但不一定是针对初始非自身抗原的特异性T细胞。换句话说,在正在进行的免疫反应中,非特异性抗原的T细胞可以被细胞因子作为旁观者激活,这种现象称为“旁观者T细胞激活”。然而,这一过程的高成本可能导致“表位扩散(epitope spreading)”,即宿主细胞的附带损伤导致新抗原的释放,并激活微环境中的T细胞,从而引发自身免疫。尽管普遍认为旁观者记忆T细胞的激活依赖于细胞因子,但有证据表明,自身肽/MHC复合体与细胞因子共同参与了初始T细胞的激活。在本文中,我们将深入探讨旁观者T细胞激活的机制,并讨论其在自身免疫、癌症、移植、微生物感染和动脉粥样硬化等疾病中的生物学意义。图1. T细胞旁观者激活的类型。(A) 1)抗原特异性免疫反应和/或2)抗原提呈细胞的先天刺激导致3)细胞因子/趋化因子波,4)激活旁观者T细胞,通过效应分子(颗粒酶/穿孔素)和NK受体-配体相互作用(NKG2D/NKG2DL)引起宿主细胞损伤。(B) 5)损伤可以释放新的自身抗原,这一过程被称为表位扩散,它反过来激活交叉反应性T细胞,包括最初的抗原特异性T细胞,使其成为自身反应性T细胞。02旁观者T细胞激活的机制人体内不同细胞类型之间的通讯主要受两个过程的调控:1)受体-配体相互作用;2)可溶性介质。同样,T细胞可以通过其T细胞受体(TCR)与由抗原呈递细胞(APC)呈递的肽/MHC复合体相互作用(受体-配体复合体)和/或包括细胞因子和微生物产物在内的可溶性介质激活,这两种通讯方式都可以促进T细胞的旁观者激活。旁观者T细胞激活被定义为非特异性抗原的T细胞激活。换句话说,在病毒感染期间,可能会激活不针对病毒抗原的T细胞。例如,在小鼠淋巴细胞性脉络膜炎病毒(LCMV)感染期间,已发现激活非特异性抗原的T细胞。2.1 通过可溶性介质与交叉反应性激活旁观者T细胞旁观者T细胞激活实际上可以通过两种机制发生:·首先,通过激活交叉反应性TCR(图1B);·其次,由于对原始外源抗原的强烈免疫反应,通过包括细胞因子在内的可溶性介质激活(图1A)。尽管旁观者T细胞激活现象广泛与通过可溶性介质(包括细胞因子)的刺激相关,但后续研究显示,肽段-MHC/TCR相互作用也参与其中。这些研究促使我们进一步了解调控此过程的机制,以及每种机制对T细胞亚群(初始T细胞与记忆T细胞)的不同需求。此外,我们希望澄清交叉反应性的概念及其与旁观者T细胞激活的关系。简单来说,交叉反应性是指单个TCR能够识别多个肽段-MHC复合体的能力,这一假设最初由Matzinger和Bevan提出。可以想象,免疫系统可能具有这种TCR退化特性或所谓的异源免疫,以识别大量微生物表位,但分子模拟可能是这种能力的高成本,导致自身和非自身表位之间的重叠,从而引发针对自身的免疫反应并发展为自身免疫疾病。一个典型的例子是风湿性心包炎,其中心脏肌球蛋白与A组链球菌(GAS)相关的毒力因子M蛋白交叉反应。可以推测,宿主对细菌的免疫反应通过暴露肌球蛋白等新表位而损伤心脏组织。因此,初始T细胞免疫反应变得对自身蛋白具有交叉反应性,从而引发自身免疫(图1B)。此外,我们将讨论许多自身免疫疾病的特征,即在炎症/受损器官中存在旁观者激活的非特异性抗原T细胞,表明它们的激活可能是通过促炎性微环境和/或交叉反应性发生的。然而,区分通过细胞因子与交叉反应性的旁观者T细胞激活是具有挑战性的,因为TCR对自身具有一定的响应性,即tonic 信号。在以下部分中,我们将讨论调控旁观者T细胞激活的机制及其对初始和记忆CD8 T细胞的影响。2.1.1 微生物产物和细胞因子在初始和记忆T细胞激活中的作用细胞因子在特定微环境中的分泌以及病原体相关分子模式(PAMPs)的作用是两个相互关联的过程,PAMPs的激活会导致细胞因子的分泌。因此,模式识别受体(PRRs)的表达上调。已知PAMPs可以直接通过PRRs(包括Toll样受体(TLRs))与T细胞结合,作为共刺激信号,激活它们上调激活标志物和细胞因子的分泌。例如,TLR2在T细胞中的激活可以增强其效应功能和存活,而TLR7在T细胞中的激活对实验性自身免疫性脑脊髓炎的发病机制有贡献。在体外用Burkholderia pseudomallei细菌感染脾细胞,与初始CD8 T细胞(CD44lo)相比,激活/记忆CD8 T细胞(CD44hi)中IFNγ的表达迅速增加。此外,Sprent实验室表明,记忆T细胞对TLR配体(包括poly I:C(TLR3配体)和LPS(TLR4配体))有反应,这些配体可以诱导I型干扰素,从而通过上调IL-2/IL-15Rb(CD122)使记忆CD8 T细胞对IL-15和IL-2产生反应。为了进一步研究PAMPs对体内T细胞旁观者激活的作用,向初始小鼠中注射poly I:C以模拟病毒感染,结果发现多克隆记忆CD8 T细胞在TCR独立的方式下增殖。几项研究探讨了促炎细胞因子(如IL-12和IL-18)以及共同γ链细胞因子IL-15对旁观者T细胞激活的影响(图2B)。例如,IL-12和IL-18的组合可诱导记忆CD8 T细胞的增殖和IFNγ表达。此外,IL-12通过增强IL-18R的表达来增强T细胞中IFNγ的诱导。此外,IL-15在没有TCR刺激的情况下可激活记忆CD8 T细胞增殖并获得效应功能,而长期暴露可增强其细胞毒性,即上调穿孔素、颗粒酶、CD107a、颗粒溶解素和NK受体(如NKG2D)。NKG2D可以在没有TCR刺激的情况下介导直接细胞杀伤,识别其配体,包括人类中的应激诱导蛋白MICA和MICB,以及小鼠中的H60和Mult1,这种结合通过DAP10/12激活下游信号传导。靶细胞的杀伤可能导致自身抗原的释放,从而通过表位扩散激活旁观者T细胞,放大自身免疫反应(图1A, 3A, 4A)。例如,在乳糜泻(一种自身免疫疾病)中,肠上皮细胞表达IL-15,这上调了浸润肠内的T细胞上的NKG2D,使它们能够靶向肠上皮细胞,导致损伤,并可能释放自身抗原,激活T细胞并放大旁观者T细胞反应。IL-15还可调节旁观者记忆CD8 T细胞向炎症部位的迁移。在急性甲型肝炎期间,IL-15上调CCR5趋化因子受体,增强其对肝实质的需求(图3A)。细胞因子之间的协同作用在旁观者T细胞激活中起着重要作用,例如,IL-23和IL-1b可以协同诱导效应/记忆CD4 T细胞中IFNγ、IL-22和GM-CSF的表达。另一个细胞因子协同作用和旁观者激活的例子是IL-2和IL-33,事实上IL-2在Th2 CD4 T细胞中上调IL-33R(ST2),使其表达IL-13。此外,IL-1家族的促炎细胞因子IL-18可以以抗原独立的方式诱导初始和记忆CD4 T细胞中IFNγ的表达以及Th17 CD4 T细胞中IL-17的表达。在IL-18的刺激下,IL-18Ra+记忆CD4 T细胞表达多种细胞因子,包括IL-5、IL-6、IL-13、IL22、GM-CSF、TNFα和IFNγ。IL-12对IL-18Ra的上调可以归因于IL-12,它与IL-18协同作用,诱导Th1和Th17在TCR独立的方式下表达IFNγ。最后,高剂量的IL-2可以克服TCR刺激的需求,使初始CD4 T细胞对IL-12和IL-18产生反应,并获得Th1表型和表达IFNγ。化疗和放疗后的淋巴细胞减少症是细胞因子的另一个来源,在这些情况下,T细胞池显著减少。因此,包括IL-7和IL-15在内的稳态细胞因子的生物可用性增加,导致T细胞的扩增,这一过程称为淋巴细胞减少症诱导的稳态增殖(LIP)。对于初始CD8 T细胞而言,它们可以在淋巴细胞减少症的条件下通过自身肽段/MHC依赖的方式增殖并获得记忆样表型和功能,而无需非自身抗原(图2A)。在稳态条件下,初始CD8 T细胞在IL-15和转录因子EOMES的存在下也可以获得记忆样表型。这些未经历抗原的细胞被称为“虚拟记忆”T细胞(TVM),它们在衰老过程中积累。后来研究表明,经历LIP的初始T细胞在表型上与TVM非常相似。总的来说,这些研究显示了细胞因子和持续TCR刺激在初始CD8 T细胞激活中的重要性。因此,我们推测初始T细胞也可以经历另一种旁观者激活,与记忆CD8 T细胞不同,即依赖于细胞因子和自身肽段/MHC复合体。这种不同需求可能归因于每种T细胞亚群在发育过程中获得的特定表观遗传程序,使记忆T细胞比初始CD8 T细胞更容易快速回忆效应反应。事实上,与初始CD8 T细胞相比,人类记忆CD8 T细胞在稳态增殖期间保持效应分子和细胞因子(如IFNγ和Prf1)启动子区域的开放未甲基化状态。此外,初始CD8 T细胞在经典的体外TCR/CD28刺激下无法表达IFNγ,即使在存在共同γ链细胞因子的情况下。然而,它们在抗CD3/CD28抗体和促炎细胞因子IL-12的存在下上调激活标志物CD38并表达IFNγ。图2. 旁观者激活记忆T细胞与初始T细胞的稳态增殖。(A)在淋巴细胞减少的情况下,幼稚的CD8 T细胞识别MHC-I呈递的自身抗原,对IL-2和交叉呈递的IL-15水平的增加作出反应。它们获得增殖效应/记忆样表型。(B)抗原特异性幼稚T细胞识别递呈MHC的特异性抗原。同时,被活化的抗原呈递细胞交叉呈递的IL-15以及IL-12和IL-18,以不依赖于TCR的方式激活旁观者记忆T细胞。激活的记忆细胞上调自然杀伤组2D受体(NKG2D),并产生高水平的效应分子/细胞因子,包括IFNγ以及颗粒酶和穿孔素。2.1.2 肽段/MHC复合体在初始和记忆T细胞激活中的作用如前所述,初始CD8 T细胞可以在淋巴细胞减少条件下增殖并上调T细胞激活标志物(图2A),这表明细胞因子在LIP中的重要性。然而,它们仍然需要与自身肽段MHC复合体相互作用。例如,通过FACS纯化的P14初始CD8 T细胞(LCMV抗原特异性CD8 T细胞)被转移到经过照射的MHC-I缺陷小鼠中,与野生型小鼠相比,未能诱导这种增殖和激活。此外,Cho等研究表明,与野生型小鼠相比,初始CD8 T细胞在被转移到经过照射的MHC-I KO和TAP-1 KO小鼠中时未能发生增殖。这些发现表明,自身肽段/MHC-I复合体是驱动初始T细胞增殖和激活所必需的,暗示自身肽段/MHC复合体与对细胞因子的响应之间存在联系。事实上,Stoklasek等研究表明,即使在IL15/IL15Ra治疗后,将初始OT-1 CD8 T细胞转移到经过照射的MHC-I缺陷小鼠中,这些细胞也无法增殖,表明MHC-I相互作用对于初始CD8 T细胞对IL-15的适当响应是必要的。同样,LCMV急性感染导致CD8 T细胞中CD122(IL-2/IL-15Rb)的上调。上述观察结果为我们提供了自身肽段/MHC-TCR轴可能通过敏化初始细胞以响应共同γ链细胞因子的线索。尽管细胞因子在记忆T细胞的旁观者激活中起着明确的作用,但Goplen等研究表明,在记忆T细胞的旁观者激活后,TCR下游信号通路被激活。事实上,通常驱动旁观者记忆T细胞激活的促炎细胞因子(如IL-12、TNFα和IL-15)导致CD3e链的磷酸化,进而传播TCR下游的信号通路,包括ZAP70及其下游信使LAT。因此,该研究表明促炎细胞因子利用TCR/CD3信号体来促进旁观者效应/记忆CD8 T细胞反应。为了阐明MHC在记忆CD8 T细胞旁观者激活中的作用,作者将VSV特异性CD8记忆T细胞转移到MHC-I充足或缺陷的同系小鼠中,随后感染无关病原体(李斯特菌)。结果显示,在MHC-I缺陷小鼠中IFNγ的表达减少。这些数据表明MHC-I在记忆CD8 T细胞的旁观者激活中起着重要作用。一个显而易见的问题是:“这些细胞是否能抵抗无关感染?”一个直接的实验是将抗原特异性记忆T细胞转移到初始小鼠中,随后感染无关病原体。例如,Soudja等研究表明,将来自感染李斯特菌-Ova小鼠的LCMV多克隆记忆CD8 T细胞或OT-1记忆CD8 T细胞过继转移到野生型小鼠中,可以减少李斯特菌的细菌负荷。同样,Berg等观察到使用表达Ova的 vaccinia 病毒作为初次感染可以抵抗李斯特菌。03旁观者T细胞激活的生物学意义尽管旁观者T细胞激活在人类和多种小鼠模型中被广泛描述,但旁观者T细胞的功能可能因疾病而异,即保护性或致病性。此外,其他研究未观察到该过程对病原体清除的显著贡献。这可能归因于其他细胞类型(包括γδ T细胞、ILCs和非传统记忆T细胞)对正在进行的免疫反应的掩盖效应。关于旁观者T细胞功能缺乏共识可能源于使用不同的临床前实验小鼠感染模型,在接下来的部分中将讨论旁观者T细胞激活在病原体免疫应答以及癌症、动脉粥样硬化、自身免疫和移植中的作用。3.1 旁观者T细胞在微生物感染中的作用旁观者T细胞激活在人类传染病中已有充分记载,例如在原发性人类免疫缺陷病毒(HIV)和乙型肝炎病毒(HBV)感染患者中,不仅检测到抗原特异性CD8 T细胞的强烈激活,还检测到EBV、CMV和流感特异性CD8 T细胞的激活。此外,HIV患者在中断抗逆转录病毒治疗后,表现出抗原特异性和非特异性CTLs的激活。这些观察结果被归因于共同γ链细胞因子IL-15在旁观者T细胞的扩增和激活中的作用。然而,一个仍然存在的问题是:“这些旁观者T细胞在感染中起什么作用?”是保护性还是致病性?在HBV的情况下,旁观者激活的CD8 T细胞可能不参与HBV清除,但与病毒性肝炎相关的免疫病理学有关。这些细胞促成了慢性病毒性肝炎的特征——肝实质损伤。同样,急性甲型肝炎病毒(HAV)感染与严重的肝实质损伤相关,这被认为是由HAV特异性CD8 T细胞引起的(图3A)。然而,在黑猩猩中,HAV特异性CD8 T细胞在用HAV特异性肽段刺激后未能产生显著水平的IFNγ或CD107a,表明病毒特异性CTLs功能低下。为了进一步了解CD8 T细胞在HAV感染中的作用,Kim等评估了急性HAV感染期间激活的CD8 T细胞的特异性。他们发现,在急性HAV感染患者的外周血中,大量激活的CD38+ HLA-DR+ CD8 T细胞与HAV无关,而是针对流感、EBV、CMV、痘病毒和呼吸道合胞病毒,这与HIV和HBV患者的早期观察结果相呼应。此外,旁观者CMV和EBV特异性CD8 T细胞的激活与儿童急性戊型肝炎相关。此外,外周血中多克隆Th1 CD4 T细胞和CD8 T细胞的频率增加。这些观察结果提出了一个问题:“非认知抗原特异性‘旁观者’T细胞扩增和激活的机制是什么?”在急性HAV和HEV感染患者的血清中观察到IL-15和IL-18水平升高,表明这些细胞因子在激活无关病毒特异性CD8 T细胞方面发挥作用。此外,用HAV感染人类肝癌细胞系(HepG2)导致高水平IL-15的产生,这已被证明可以在没有认知抗原刺激的情况下驱动HAV无关的CD8 T细胞激活(NKG2D上调)。为了评估这些旁观者激活的CD8 T细胞在诱导肝脏组织损伤中的作用,作者显示,从健康对照组分离的IL-15激活的CD8 T细胞和从急性甲型肝炎(AHA)患者肝脏中分离的肝内CD8 T细胞能够裂解不表达MHC I类的K562靶细胞,以及肝源性Huh-7细胞。此外,从AHA患者外周血分离的CMV特异性CD8 T细胞(而非健康成人)能够裂解K562细胞。这些结果表明,与AHA感染相关的肝损伤是TCR独立的,并且可以通过IL-15激活的HAV无关CD8 T细胞以NKG2D依赖的方式发生。事实上,该小组能够推断出激活的HAV无关病毒特异性CD8 T细胞的比例与急性甲型肝炎感染期间肝脏组织损伤之间存在正相关。另一个显示旁观者T细胞激活对病毒感染贡献的例子是拉沙病毒引起的动物源性病毒性出血热,该病毒在西非流行。使用骨髓嵌合小鼠模型随后进行拉沙病毒感染,作者证明了多克隆CD8 T细胞以及OT-1细胞(卵清蛋白特异性)的激活。同样,在无症状或轻度症状的COVID-19患者中,与重度症状患者相比,出现了COVID-19非特异性的CD8 T细胞爆发(图3B)。这种早期旁观者CD8 T细胞的扩增可能在防止疾病进展中发挥作用,在COVID-19早期利用这种非特异性反应可以成为避免疾病进展的更好策略。这项工作提供了旁观者激活T细胞在疾病免疫病理学中作用的近距离机制见解。图3. 微生物感染期间旁观者T细胞的活化。(A)甲型肝炎病毒(HAV)感染肝细胞导致IL-15的释放,IL-15激活非特异性“旁观者”CD8 T细胞,包括EBV和CMV特异性(以不同颜色描绘)。这些活化的T细胞通过NKG2D和细胞毒性细胞因子/分子(包括穿孔素、颗粒酶和IFNγ)对肝细胞造成损伤。整体肝细胞损伤可能导致释放新的自身抗原,激活T细胞并通过“表位扩散”(虚线箭头)引起自身免疫。(B)无症状/轻度COVID-19患者的特点是旁观者t细胞激活的早期爆发,这可能保护他们免受疾病进展到严重的临床表现。3.2 旁观者T细胞在癌症中的作用人们普遍认为,肿瘤浸润性T细胞(TILs)在特异性上具有异质性,即同时包含肿瘤特异性和非特异性T细胞,其中肿瘤抗原特异性CD8 T细胞(CTLs)在TILs中的比例因肿瘤类型而异。例如,黑色素瘤肿瘤的TILs中可能包含50%-80%的肿瘤反应性CTLs。另一方面,冷肿瘤(如浆液性卵巢癌和微卫星稳定型结直肠癌)的TILs缺乏肿瘤反应性T细胞库。这些肿瘤的TILs中包含一些病毒特异性T细胞,如EBV反应性CD8 T细胞。同样,胶质母细胞瘤、肾细胞癌、子宫内膜癌、头颈部、甲状腺和乳腺癌中也存在EBV、CMV和流感特异性记忆CD8 T细胞。3.2.1 旁观者CD8 T细胞的招募这些旁观者CD8 T细胞被招募到肿瘤微环境中的主要驱动因素是肿瘤生态位中富集的趋化因子和炎症线索,且这一过程与认知抗原无关。肿瘤细胞可以分泌趋化因子,如CCL5。接下来,由IFNγ刺激的抗原呈递细胞产生的CXCL9招募表达CXCR3的T细胞。CXCL10也参与了招募CXCR3+ T细胞的过程,这些T细胞大多为旁观者。然而,肿瘤特异性T细胞也可以表达两种趋化因子受体(CXCR3和CCR5),这表明旁观者T细胞的招募仅仅是伴随肿瘤特异性T细胞招募的一个附带现象。在这两种情况下,旁观者T细胞都会浸润并积聚在肿瘤中。3.2.2 利用旁观者T细胞的方法在多种肿瘤中检测到未耗竭的病毒特异性T细胞,并且它们与更好的肿瘤控制相关,这促使人们考虑利用它们的细胞毒性,特别是由于许多肿瘤抗原是自身或修饰的自身抗原,无法引发强烈的TCR刺激。3.2.2.1疫苗和感染小鼠模型一种实现这一目标的方法是通过用表达OVA的VSV感染携带同系OT-1 CD8 T细胞的野生型初始小鼠来建立OT-1嵌合体。这一方法在感染后30天以上诱导OT-1记忆CD8 T细胞反应。向肿瘤负荷小鼠中注射VSV病毒肽可重新激活OT-1记忆T细胞,这与B16黑色素瘤生长的延迟相关。此外,对肿瘤负荷小鼠进行全身性抗PD-L1抗体治疗,同时在肿瘤内注射VSV-OVA肽,可在34%的小鼠中根除B16肿瘤。这些数据表明,激活旁观者记忆病毒特异性T细胞可以增强抗肿瘤免疫。这种效果通过PD-L1阻断进一步增强,事实上,使用PD1 KO小鼠模型或阻断PD-1/PD-L1轴可以增强旁观者T细胞的功能,但会降低T细胞的寿命。同样,用灭活的流感病毒进行肿瘤内治疗可减少肿瘤生长并增加CD8 T细胞的浸润。这种治疗被证明可以使“冷”非免疫原性肿瘤对检查点免疫疗法敏感,使其成为“热”且响应性的肿瘤。即使在转录组水平上,Caushi等也显示,在接受免疫检查点阻断治疗的肺癌患者的肿瘤组织中,病毒特异性CD8 T细胞富集,这些病毒特异性CD8 T细胞表达的效应基因比肿瘤特异性CD8 T细胞更高。这些结果表明,感染和癌症的同时发生可以通过TCR独立的方式激活肿瘤微环境中的预先存在的病毒特异性CD8 T细胞。3.2.2.2细胞因子和嵌合抗原受体T细胞方法另一种激活旁观者T细胞的方法是通过基于细胞因子的免疫疗法和嵌合抗原受体(CAR)T细胞。事实上,向携带肿瘤的小鼠(B16、3LL或Renca)注射抗CD40/IL-2,可以显著扩增记忆CD44hi NKG2D+ CD8 T细胞,并产生显著的抗肿瘤效果。最近研究表明,CTLs可以通过NKG2D-NKG2DL轴杀死下调MHC-I的肿瘤细胞。此外,基于IL-15的超级激动剂(ALT-803)可以富集表达NKG2D的先天样CD8 T细胞,这些细胞具有抗肿瘤活性,且与抗原无关。在体内,ALT-803可以清除骨髓中的骨髓瘤,为治疗小鼠提供生存益处。这些研究表明,抗肿瘤效应可以通过基于细胞因子的免疫疗法诱导,并且由扩增的NKG2D+记忆CD8 T细胞以MHC独立的方式介导。此外,CAR T细胞可以设计为同时靶向CD3链和广泛表达的肿瘤抗原(如EphA2),后者常见于胶质母细胞瘤、肺癌、乳腺癌和前列腺癌。因此,这些“接合”细胞不仅靶向肿瘤,还可以激活旁观者T细胞。同样,使用单细胞RNA测序方法,Kaminski首次展示了在B细胞白血病CAR治疗后,CARneg CD8旁观者T细胞的转录组特征富含NK样标记(CD160、KLRD1和KIR3DL2)以及趋化因子和趋化因子受体(CCR9和CCL5),而初始特征较少。这里一个显而易见的问题是:“旁观者CD4 T细胞是否有任何作用?” CD4和CD8是否可以协同增强肿瘤杀伤?Lee等很好地讨论了旁观者CD4 T细胞在感染、自身免疫和癌症中的作用。此外,Joncker等将能够识别HY雄性抗原的TCR转基因CD4和CD8 T细胞共同注入携带纤维肉瘤肿瘤的雌性小鼠中。在用雄性细胞对小鼠进行初次免疫后,CD4和CD8 Tg T细胞在肿瘤和肿瘤引流淋巴结中积聚和扩增,被认为是旁观者。此外,Schietinger等使用转基因小鼠模型表明,CD4和CD8 T细胞的协作是旁观者肿瘤细胞杀伤的必要条件。综上所述,上述研究提示,在小鼠和人类中,旁观者CD4和CD8 T细胞在肿瘤浸润性T细胞(TILs)中对肿瘤免疫有积极贡献。3.3 旁观者T细胞与自身免疫和同种异体免疫自身免疫和同种异体免疫反应被视为同一枚硬币的两面。在自身免疫性疾病中,免疫反应失调,导致自身反应性T细胞的持续存在和激活,从而引发疾病后果。然而,自身免疫的初始事件和传播机制仍不十分清楚。在同种异体免疫的情况下,移植物排斥是由识别供体器官中的非自身抗原引起的。因此,这两种免疫反应都是由于自身耐受的破坏,但其背后的原因不同。一种是通过缺失自身导致自身免疫的发展,而在移植物排斥的情况下,它是对供体移植物中非自身抗原的识别。3.3.1 旁观者T细胞在自身免疫性疾病中的作用在由感染、疫苗接种甚至同种异体抗原介导的强烈免疫反应期间,旁观者激活逃避免 Holtsmark筛选的低亲和力自身反应性CD8 T细胞似乎是自身免疫的一种合理假设,这一假设在过去的几十年中得到了评估和研究。例如,这可以解释在疫苗接种或实体器官移植后自身免疫性疾病的发作或复发。旁观者激活对自身免疫疾病发病机制的贡献源于早期关于疱疹性巩膜炎(HSK)的临床前小鼠模型的工作,这是一种由HSV-1引起的角膜感染导致的自身免疫性疾病。HSV-1感染的OVA转基因RAG−/−或SCID小鼠的TCR仅对OVA肽有反应,却导致了HSK。这些结果表明自身免疫不需要TCR介导的激活,并证明了T细胞的激活超出了抗原特异性。图4. 自身免疫性疾病中旁观者T细胞的激活。(A)髓磷脂特异性和非髓磷脂特异性T细胞通过促炎细胞因子参与多发性硬化症期间神经元髓鞘的损伤。新的自身抗原的释放可能会通过激活对原始抗原不具有特异性的T细胞而加重疾病。(B)柯萨奇病毒和其他病毒可以通过几种方式触发和促进胰岛素分泌β细胞的损害。此外,先天样的旁观者T细胞如iNKT、MAIT和gd T细胞也在T1D中起致病作用。(C)滑膜中的大多数T细胞是抗原非特异性的,包括EBV和CMV特异性,通过分泌促炎细胞因子对滑膜造成损伤。(D)血管内壁的动脉粥样硬化斑块富含载脂蛋白特异性和非特异性T细胞。3.3.1.1多发性硬化症多发性硬化症(MS)主要是由自身免疫介导的中枢神经系统神经元脱髓鞘引起的,疾病复发或恶化与最近的微生物感染有关。尽管传统上认为主要是由激活的髓鞘蛋白自身反应性T细胞(如髓鞘少突胶质细胞糖蛋白(MOG)特异性T细胞)驱动,这些T细胞与微生物表位交叉反应,但最近对实验性自身免疫性脑脊髓炎(EAE)小鼠模型的研究表明,旁观者激活的自身反应性T细胞是MS发病机制的另一种机制。例如,大多数浸润中枢神经系统的CD4 T细胞并非针对MOG,它们主要表达与Th17细胞相关的细胞因子,包括IL-17A、IFNγ和GM-CSF(图4A),Tregs可以抑制这些细胞。Kim等表明,工程化的髓鞘碱性蛋白(MBP)特异性Tregs有能力不仅抑制抗原特异性T细胞,还能抑制非特异性T细胞。此外,其他研究表明Tregs可以以抗原独立的方式抑制T细胞。显而易见的问题是:“这些细胞如何在TCR独立的方式下被激活?” IL-1家族成员IL1β可以诱导CD4 T细胞表达GM-CSF和转录因子Bhlh40。此外,从MS患者分离的CD4 T细胞表达IL-1R1以及TLR2和TLR4,这些受体也有助于产生IL-6、IL-17A、IFNg和GM-CSF。Nogai等表明,在CD4 T细胞模型中,用LPS处理仅识别MBP Ac1-11肽的转基因小鼠会导致EAE的发作。有趣的是,其他实验室表明,CD4旁观者T细胞也可以发挥神经保护作用。这种保护主要由IL4介导,表明Th2介导的免疫反应可能对EAE具有保护作用。此外,IL-12家族成员IL-27可以诱导CD4 T细胞中PD-L1的表达,从而改善EAE。由于正在进行的免疫反应导致的宿主细胞损伤可能导致新自身抗原的释放,这一现象称为表位(决定簇)扩散。自身抗原的识别导致自身免疫,例如,在复发-缓解型实验性自身免疫性脑脊髓炎(R-EAE)中,表位扩散在疾病恶化中起着关键作用,其中T细胞最初由特定的免疫优势表位激活,如PLP或MBP。然而,中枢神经系统的损伤暴露了原本未被靶向的额外髓鞘表位(分子间表位扩散)。另一方面,分子内表位扩散发生在同一蛋白内,在这种情况下,自身抗体可以结合到与初始结合不同的蛋白区域。此外,与健康对照相比,1型糖尿病患者中存在多种胰腺组织抗原GAD-65和胰岛素原,支持分子内表位扩散。3.3.1.2 1型糖尿病1型糖尿病(T1D)的特征是自身反应性T细胞损害胰岛素分泌的胰腺朗格汉斯岛β细胞。尽管该疾病的初始触发因素尚未完全明确,但由柯萨奇病毒等病毒介导的感染(图4B)可以通过以下方式促成β细胞破坏:a)直接感染β细胞;b)炎症细胞因子;c)分子模拟,其中病毒表位与自身抗原重叠。大多数T细胞存在于岛细胞中,是“旁观者”,不针对岛抗原,主要通过减少抗原特异性T细胞对自身抗原的可及性发挥保护作用。此外,几项研究表明,在T1D中,包括MAIT、γδ T细胞和iNKT细胞在内的先天样T细胞具有致病性(图4B)。3.3.1.3类风湿性关节炎有人提出,在包括类风湿性关节炎(RA)和乳糜泻在内的广泛自身免疫疾病中,CD8 T细胞的旁观者激活。事实上,在类风湿性关节炎患者的滑液中检测到EBV和CMV特异性激活的CD8 T细胞(图4C)。这些无关CD8 T细胞的激活被认为是由富含滑液环境的慢性炎症环境介导的。事实上,TLR2的激活通过T细胞IFNγ分泌启动RA,无需特定抗原。此外,细菌脂多糖可以激活破骨细胞,促进促炎环境。尽管研究表明,表达TLR4的CD8 T细胞与疾病严重程度和效应细胞因子/分子的表达相关,但其他报告建议它们具有调节功能。关于CD4 T细胞,NKG2D+ CD4 T细胞在RA患者的外周血和滑膜中富集。NKG2D配体MICA/B在响应包括TNFα在内的促炎细胞因子时在滑膜中上调,暗示NKG2D/NKG2DL轴在关节损伤中的作用。RA可以在另一种临床前自身免疫疾病模型(干燥综合征)中发展,表明旁观者T细胞激活可能通过交叉反应性发生;然而,作者并未排除这种可能性。3.3.1.4动脉粥样硬化在过去几年中,自身免疫在动脉粥样硬化(一种以富含脂质和免疫细胞的动脉壁斑块为特征的常见病理,构成心血管疾病的基础)的发病机制中的重要性已被广泛接受。事实上,动脉粥样硬化患者携带针对含载脂蛋白B的脂蛋白(如LDL)的循环自身抗体,这表明自身耐受的丧失。这实际上促使几个实验室努力理解动脉粥样硬化期间的自身免疫机制。例如,Wang和Depuydt等的研究利用单细胞RNA测序和TCR测序表明,在动脉粥样硬化中,外周耐受性被破坏。在Wang等的小鼠研究中,斑块特异性T细胞在细胞毒性CD8 T细胞室中扩增程度最高,这些细胞表达CD69和Fosb,均表明TCR信号传导。类似观察结果在冠状动脉疾病(CAD)患者中也有记录。此外,在Apoe−/−小鼠动脉粥样硬化模型中,主动脉斑块内的大多数CD8 T细胞克隆与主动脉引流淋巴结(RLNs)中的T细胞克隆共享TCR模式。其他研究表明,在小鼠和动脉粥样硬化患者中存在ApoB特异性CD4 T细胞(图4D)。尽管上述研究表明动脉粥样硬化具有自身免疫性质,但自身免疫的触发因素尚未完全明确。然而,文献中最近的一些观察结果可能解释这一现象。例如,感染发作与CAD并发症相关。这一过程可能涉及动脉粥样硬化斑块中的CD8细胞。这些细胞中的一小部分显示出对流感病毒、EB病毒(EBV)和巨细胞病毒(CMV)的交叉反应性。同样,de Jong等发现,约2%的斑块TCR序列特异性针对病毒表位,其中T细胞显示出激活迹象。为了研究这一过程是否通过分子模拟发生,作者从MHC-I分子中洗脱肽段并进行质谱分析。他们观察到几种可能交叉反应的肽段;然而,尚未测试这些肽段是否能够刺激斑块中的T细胞。另一种可能的解释是,斑块中的T细胞以抗原独立的方式被炎症期间分泌的细胞因子非特异性激活。3.3.1.5系统性红斑狼疮系统性红斑狼疮(SLE)是一种复杂的自身免疫性疾病,其特征是凋亡细胞清除缺陷,导致自身耐受的破坏和针对dsDNA的自身抗体产生,进而导致包括肾脏在内的系统器官损伤。表达NKG2D的活化旁观者CD4 T细胞分泌IL-10和TGF-β,提示其在SLE中具有免疫调节作用。此外,在体外,这些细胞可以抑制T细胞增殖。相反,尘螨主要过敏原Der p2可以上调SLE患者PBMCs中促炎细胞因子的表达,以旁观者方式激活B细胞产生自身抗体。3.3.2 旁观者T细胞在移植中的作用在移植中,旁观者T细胞激活的作用尚未广泛讨论;然而,几项研究报告了TLR激动剂和微生物感染对临床前小鼠模型中移植物排斥的显著影响。例如,Welsh等表明,尽管对胸腺切除小鼠进行耐受诱导治疗(例如,共刺激阻断,如抗CD154和供体特异性白细胞),通常可使皮肤移植物存活超过100天,但急性LCMV感染会引发移植物排斥。此外,TLR激动剂治疗可迅速导致皮肤异体移植物排斥,即使在共刺激阻断治疗下也是如此。在一项人类心脏移植血管病变(CAV)研究中,作者建议旁观者T细胞侵入移植物。04旁观者T细胞激活的治疗意义如前所述,旁观者T细胞激活可能导致病理效应或保护性效应,这取决于疾病背景。例如,急性病毒性肝炎感染与主要由旁观者T细胞介导的肝实质细胞损伤相关(图3A)。相反,旁观者T细胞的早期爆发式激活与无症状/轻度COVID-19症状相关,但在重症患者中缺失(图3B)。因此,似乎合理的是首先明确旁观者T细胞在特定疾病环境中的作用,然后决定是利用还是抑制这些细胞。尽管这两种疾病情境都是由病毒感染介导的,但尚不清楚为什么旁观者细胞在一种情况下具有保护性,而在另一种情况下则不然。可以推测,炎症环境和组织类型的差异可能起作用。由于旁观者T细胞以抗原独立的方式被激活且缺乏抗原特异性,因此难以靶向它们。然而,NK受体NKG2D可能是可靶向的表面蛋白之一。事实上,在HBV临床前小鼠模型中阻断NKG2D可减少肝脏损伤(图5)。相反,在李斯特菌感染期间,阻断NKG2D会加剧疾病,表明NKG2D+细胞特别是CD8 T细胞具有保护性。在COVID-19患者中,早期旁观者T细胞的爆发式激活现象可以被利用以避免疾病进展并诱导早期病毒控制。然而,尚不清楚为什么一组患者会出现这种早期旁观者激活,而另一组患者则不会。TILs的异质性以及NKG2D的表达可以通过多种方式被利用以增强抗肿瘤免疫,例如细胞因子诱导的杀伤细胞疗法是一种方法,其中包括IL-2和IFNγ在内的细胞因子混合物可用于上调NK细胞受体(如NKG2D)。同样,工程化白细胞介素(如IL-15以及IL-2和抗CD40的组合)可以增强扩增并诱导癌细胞杀伤,通过NKG2D以TCR独立的方式(图5)。由于肿瘤中广泛表达病原体衍生的肽段,例如表达CMV抗原的胶质母细胞瘤,而黑色素瘤富含细菌抗原,因此通过基于疫苗的免疫疗法在肿瘤微环境中利用病毒特异性旁观者T细胞可能是一种替代策略(图5)。例如,活性流感疫苗在小鼠模型和人类患者中均增强了肺癌结果。此外,研究显示,通过注射灭活的流感病毒进行肿瘤内疫苗接种显著减少了皮肤黑色素瘤并提高了生存率。具有双重TCR(一个针对肿瘤抗原,一个针对病毒特异性受体)的CAR T细胞甚至可以成为提高肿瘤杀伤效率的更好策略(图5)。图5. 旁观者T细胞在癌症、病原体控制和自身免疫中的治疗意义。在癌症中,有几种方法可以利用旁观者T细胞,包括工程细胞因子、疫苗免疫疗法和接合CAR-T细胞。阻塞NKG2D在自身免疫的情况下,针对IL-15和耐受诱导可能潜在的方法抑制旁观者T细胞,而在病原体的控制,IL-15诱导和开发疫苗可能是新颖的策略。05结论和展望抗原特异性是适应性免疫反应的标志;然而,最近在同种异体免疫反应中描述了先天记忆的存在;然而,非抗原特异性T细胞可以在炎症环境中增殖、激活并获得效应功能;后者被称为旁观者激活。旁观者激活一直被认为是记忆T细胞的另一种TCR非依赖性激活途径。对于初始T细胞而言,它们对细胞因子有反应,并且需要自身肽段-MHC结合以诱导其激活和增殖。这种现象称为稳态增殖,发生在淋巴细胞减少症条件下,如放疗诱导的骨髓消融、HIV感染以及其他诱导淋巴细胞减少的过程,可能是初始T细胞版本的旁观者激活。细胞因子需求与初始T细胞的持续TCR信号和细胞因子需求之间的差异可能归因于初始和记忆T细胞亚群在发育过程中获得的特定表观遗传程序。尽管旁观者T细胞激活的机制已被充分记录,但其功能可能因人类疾病环境或临床前动物模型而异,如我们之前讨论的微生物感染、癌症、自身免疫和移植的例子所示。为了在自身免疫的背景下利用旁观者T细胞的功能,可以从肿瘤免疫和微生物感染中汲取经验。然而,疾病环境不同,例如在癌症中,许多研究寻求利用肿瘤微环境中的旁观者T细胞的效应功能。事实上,与肿瘤特异性T细胞相比,旁观者T细胞在黑色素瘤患者中不表现出耗竭特征。然而,在自身免疫中,应开发策略以抑制自身反应性T细胞的细胞毒性或诱导耐受。与微生物感染类似,抗NKG2D可能是抑制自身免疫中旁观者T细胞的一种方法。然而,对于自身免疫,不能采用一刀切的方法,因为一些自身免疫疾病以免疫调节旁观者T细胞为特征,如在SLE中,激活的旁观者CD4 T细胞表达NKG2D并分泌IL-10和TGF-β。此外,MS中的旁观者CD4 T细胞也可以发挥神经保护作用。总之,利用旁观者T细胞进行细胞疗法代表了未来的潜在机会,其中利用肿瘤免疫是一个很好的例子。然而,在其他疾病如自身免疫的情况下,方法应根据疾病背景、组织环境以及其他因素进行量身定制。最后,旁观者T细胞可能在设计新疫苗和增强其效力方面发挥重要作用。原文链接Mechanisms governing bystander activation of T cells.Front. Immunol. 2024, 15:1465889. doi: 10.3389/fimmu.2024.1465889推文用于传递知识,如因版权等有疑问,请于本文刊发30日内联系医药速览。原创内容未经授权,禁止转载至其他平台。有问题可发邮件至yong_wang@pku.edu.cn获取更多信息。©2021 医药速览 保留所有权利往期链接“小小疫苗”养成记 | 医药公司管线盘点 人人学懂免疫学| 人人学懂免疫学(语音版)综述文章解读 | 文献略读 | 医学科普|医药前沿笔记PROTAC技术| 抗体药物| 抗体药物偶联-ADC核酸疫苗 | CAR技术| 化学生物学温馨提示医药速览公众号目前已经有近12个交流群(好学,有趣且奔波于医药圈人才聚集于此)。进群加作者微信(yiyaoxueshu666)或者扫描公众号二维码添加作者,备注“姓名/昵称-企业/高校-具体研究领域/专业”,此群仅为科研交流群,非诚勿扰。简单操作即可星标⭐️医药速览,第一时间收到我们的推送①点击标题下方“医药速览” ②至右上角“...” ③点击“设为星标
细胞疗法免疫疗法
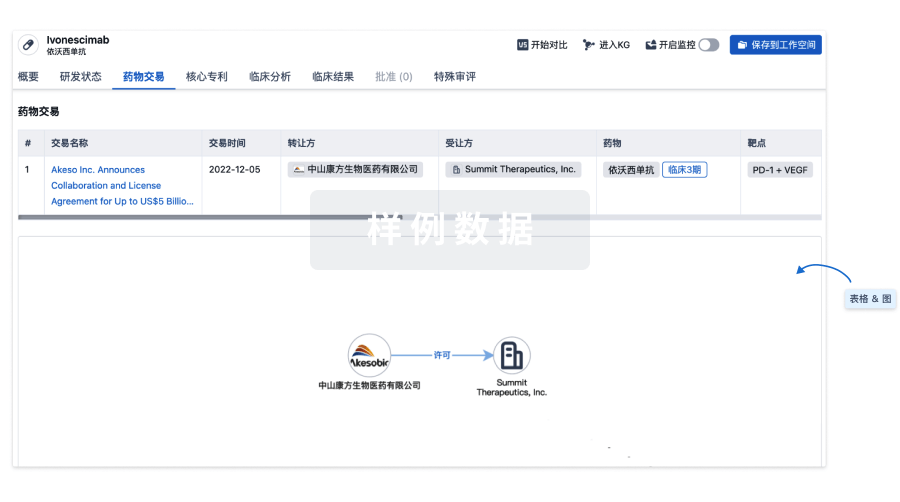
100 项与 Recombinant canarypox virus-based vaccine(Therion Biologics Corp.) 相关的药物交易
登录后查看更多信息
外链
| KEGG | Wiki | ATC | Drug Bank |
|---|---|---|---|
| - | Recombinant canarypox virus-based vaccine(Therion Biologics Corp.) | - | - |
研发状态
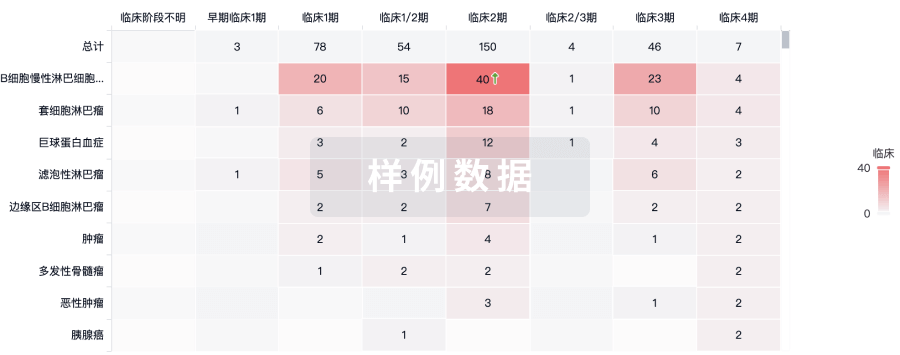
10 条进展最快的记录, 后查看更多信息
登录
| 适应症 | 最高研发状态 | 国家/地区 | 公司 | 日期 |
|---|---|---|---|---|
| 大肠腺癌 | 临床2期 | 美国 | 2017-04-05 | |
| 不能切除的大肠癌 | 临床2期 | 美国 | 2017-04-05 | |
| 转移性结直肠癌 | 临床2期 | 美国 | 2001-12-01 | |
| 转移性结直肠癌 | 临床2期 | 加拿大 | 2001-12-01 | |
| 结直肠癌 | 临床2期 | 美国 | - | |
| 结直肠癌 | 临床2期 | 美国 | - | |
| 结直肠癌 | 临床2期 | 加拿大 | - | |
| 结直肠癌 | 临床2期 | 加拿大 | - | |
| 黑色素瘤 | 临床2期 | - | - | |
| 黑色素瘤 | 临床2期 | - | - |
登录后查看更多信息
临床结果
临床结果
适应症
分期
评价
查看全部结果
| 研究 | 分期 | 人群特征 | 评价人数 | 分组 | 结果 | 评价 | 发布日期 |
|---|
No Data | |||||||
登录后查看更多信息
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
核心专利
使用我们的核心专利数据促进您的研究。
登录
或
临床分析
紧跟全球注册中心的最新临床试验。
登录
或
批准
利用最新的监管批准信息加速您的研究。
登录
或

特殊审评
只需点击几下即可了解关键药物信息。
登录
或

Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用


