预约演示
更新于:2025-05-22
CDR-132L
更新于:2025-05-22
概要
基本信息
药物类型 ASO |
别名 CDR、CDR 132L、CDR132L |
靶点 |
作用方式 抑制剂 |
作用机制 miR-132抑制剂(microRNA 132 inhibitors) |
非在研适应症 |
非在研机构- |
最高研发阶段临床2期 |
首次获批日期- |
最高研发阶段(中国)- |
特殊审评- |
登录后查看时间轴
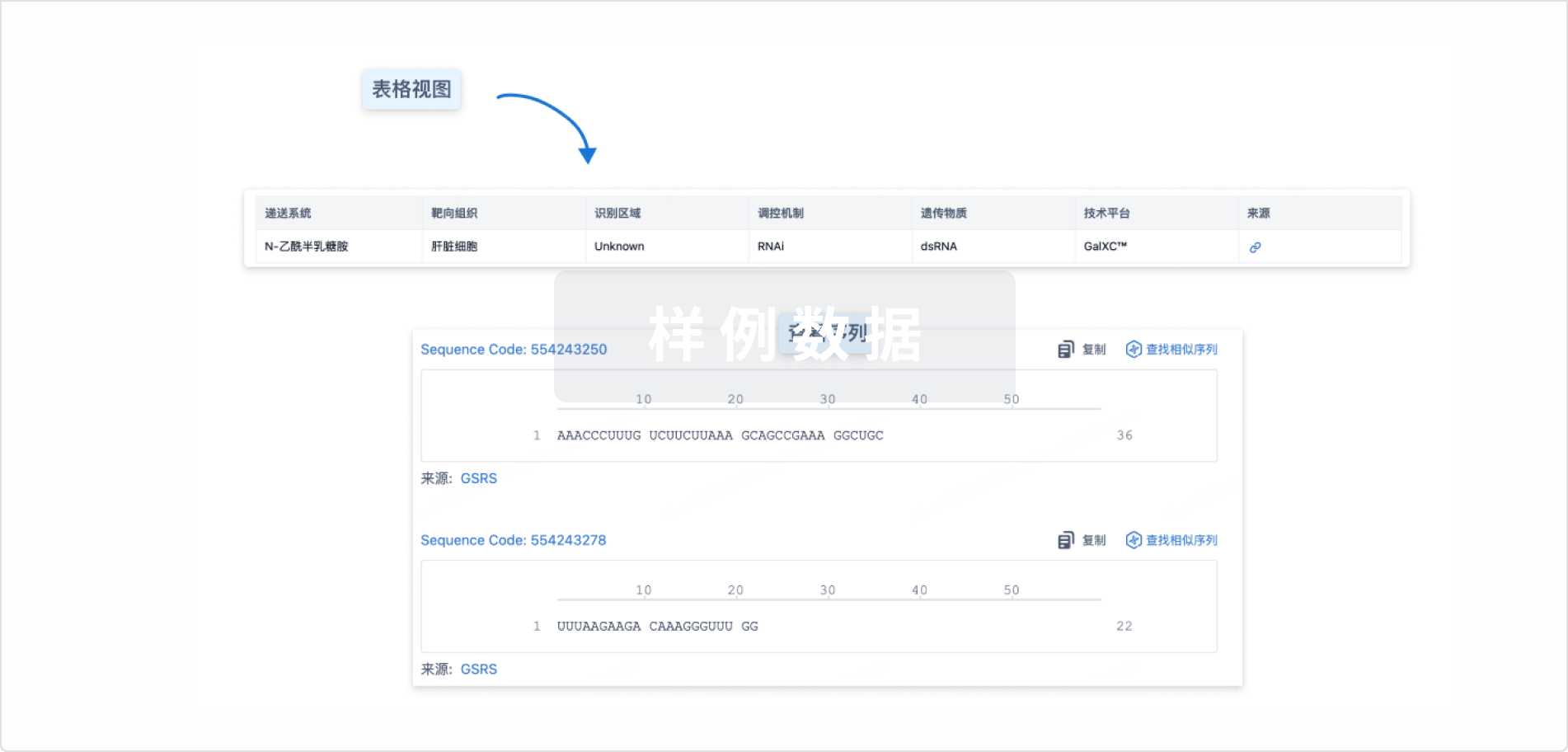
结构/序列
使用我们的RNA技术数据为新药研发加速。
登录
或
关联
4
项与 CDR-132L 相关的临床试验NCT06979375
Phase 2, Multicentre, Randomised, Double-blind, Placebo-controlled Safety and Efficacy Study of CDR132L on Reverse Cardiac Remodelling in Participants With Heart Failure With Reduced/Mildly Reduced Ejection Fraction and Left Ventricular Hypertrophy
This study will look into how CDR132L (a potential new medicine) works on the structure and function of the heart in people living with heart failure. Participants will either get CDR132L or placebo (a medicine which has no effect on the body), which treatment the participants get is decided by chance. The study will last for about 60 weeks.
开始日期2025-07-01 |
申办/合作机构 |
NCT06979362
Phase 2, Multicentre, Randomised, Double-blind, Placebo-controlled Safety and Efficacy Study of CDR132L on Reverse Cardiac Remodelling in Participants With Heart Failure With Preserved Ejection Fraction and Left Ventricular Hypertrophy
This study will look into how CDR132L (a potential new medicine) works on the structure and function of the heart in people living with heart failure. Participants will either get CDR132L or placebo (a medicine which has no effect on the body), which treatment the participants get is decided by chance. The study will last for about 60 weeks.
开始日期2025-07-01 |
申办/合作机构 |
NCT05953831
Phase 2, Multicenter, Randomized, Double-blind, Placebo-controlled Safety and Efficacy Study of CDR132L on Reverse Cardiac Remodeling in Patients With Heart Failure With Mildly Reduced or Preserved Ejection Fraction and Cardiac Hypertrophy
This is a Phase 2, multicenter, randomized, double-blind, placebo-controlled study including approximately 130 randomized HF patients with heart failure with mildly reduced or preserved ejection fraction (LVEF ≥45%), to assess efficacy and safety of CDR132L on reverse remodeling. In this study, patients with HFpEF (EF ≥50%) or HFmrEF (LVEF 45-49%) will be included.
开始日期2024-04-01 |
申办/合作机构 |
100 项与 CDR-132L 相关的临床结果
登录后查看更多信息
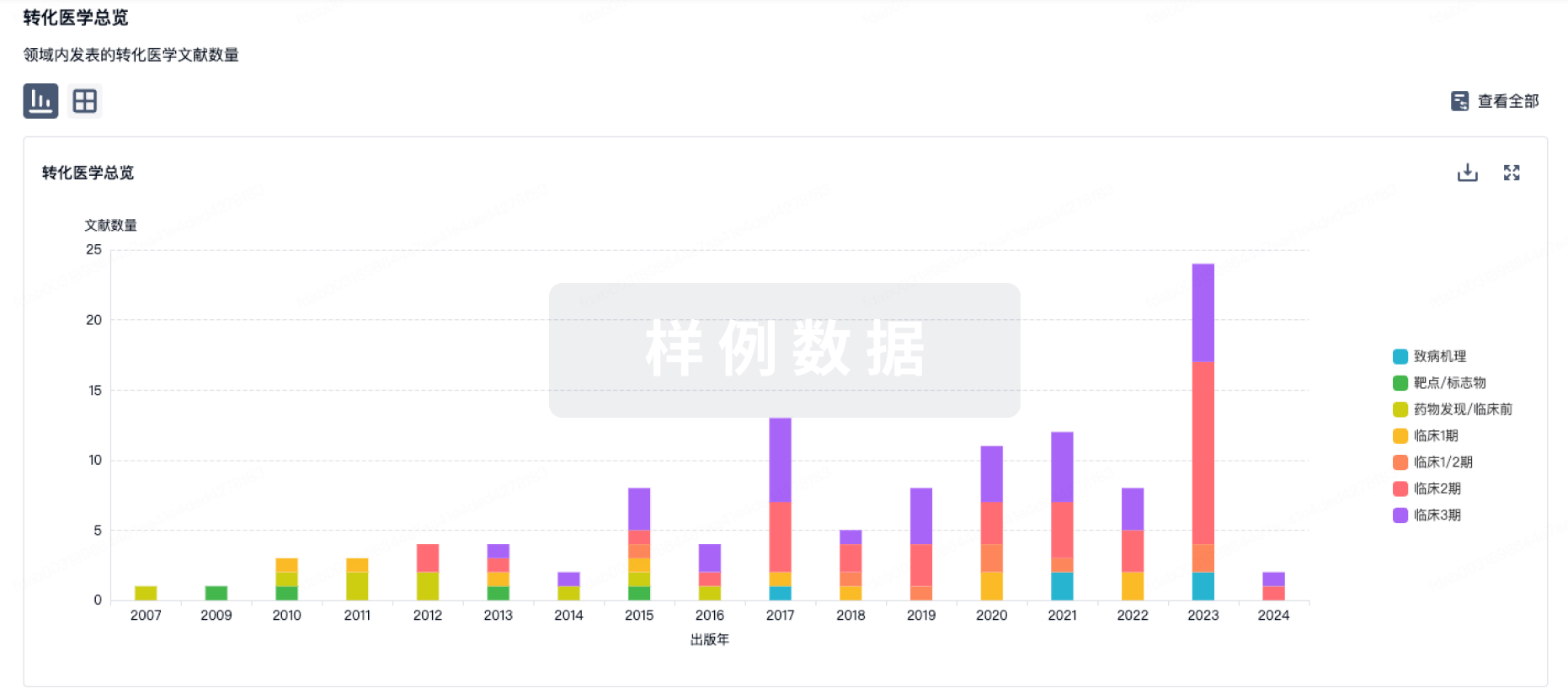
100 项与 CDR-132L 相关的转化医学
登录后查看更多信息
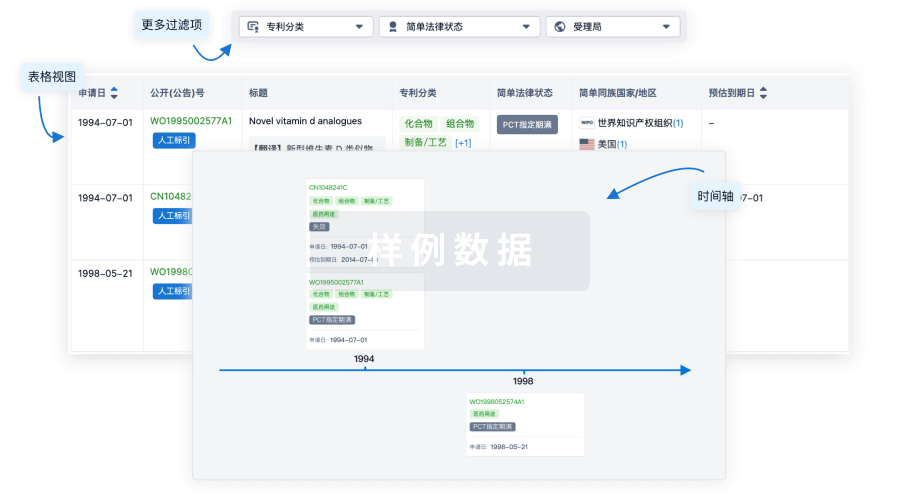
100 项与 CDR-132L 相关的专利(医药)
登录后查看更多信息
149
项与 CDR-132L 相关的文献(医药)2025-09-01·Journal of Environmental Sciences
Reduced rainfall over the Amazon basin in an idealized CO2 removal scenario: Remote dynamic processes
Article
作者: Qu, Xia ; Zhang, Suqin ; Hu, Peng ; Huang, Gang
The Amazon basin plays a crucial role in biodiversity and carbon storage, but its local rainfall is anticipated to decrease under global warming. Carbon dioxide removal (CDR) is being considered as a method to mitigate the impact of global warming. However, the specific effects of CDR on Amazon rainfall have not been well understood. Here, an idealized CDR experiment reveals that the reduced rainfall over the Amazon basin does not recover. Significantly weaker rainfall is found during the ramp-down period compared to the ramp-up period at the same CO2 concentration. This response is associated with the enhanced El Niño-like warming in the tropical Pacific Ocean during the CDR period. This warming pattern has dual effects: weakening the zonal circulation and causing anomalous descent directly over the Amazon basin, while also triggering a stationary Rossby wave train that propagated downstream and generated anomalous ascent over the Sargasso Sea. This anomalous ascent induces anomalous descent and weakens moisture transport over the Amazon basin by the local meridional circulation. Consequently, precipitation is reduced over the Amazon basin in response to the weakened zonal and meridional circulation. Our findings indicate that even if the atmospheric CO2 concentration is lowered, the Amazon basin will remain susceptible to drought. Effective local climate adaptation strategies are urgently needed to address the vulnerability of this critical ecosystem.
2025-05-01·Spine Journal
Cervical Disc Replacement in Athletes: A Modified Delphi Consensus Survey of Expert Opinion
Article
作者: Smith, Gabriel A ; Jo, Jacob ; Ludwig, Steven C ; Hecht, Andrew ; Sills, Allen K ; Hsu, Wellington K ; Cordover, Andrew M ; Nemani, Venu M ; Bonfield, Christopher M ; Feuer, Hank ; Liew, Susan M ; Maroon, Joseph ; Vaccaro, Alexander R ; Theodore, Nicholas ; Lehman, Ronald A ; Watkins, Robert G ; Chan, Patrick C H ; Louie, Philip K ; Qureshi, Sheeraz ; Rogers, Myron A ; Gardocki, Raymond J ; Cantu, Robert C ; Sasso, Rick C ; Zuckerman, Scott L ; Miele, Vincent J ; Turner, Jay D ; Rigney, Grant H ; Phillips, Frank M ; Okonkwo, David O ; Mullin, Jeff ; Levi, Allan D ; Bailes, Julian E ; Davis, Gavin A ; Joseph, Jacob R ; Riew, K Daniel ; Coric, Domagoj
BACKGROUND CONTEXT:
The safety and efficacy of cervical disc replacement (CDR) for spinal disorders in contact sport athletes is not clear. Current research is limited and highlights mixed results regarding return-to-sport (RTS) among athletes with CDR.
PURPOSE:
We sought to perform a modified Delphi consensus survey of expert opinion on CDR in athletes.
STUDY DESIGN/SETTING:
A cross-sectional, modified Delphi consensus survey of different scenarios regarding RTS for athletes with CDR was conducted among a panel of expert spine surgeons.
PATIENT/RESPONDENT SAMPLE:
An international panel of 34 spine surgeons involving both neurosurgeons and orthopaedic surgeons with sport expertise was identified.
OUTCOME MEASURES:
Consensus regarding return to any level of sport as defined above was queried as the main outcome measure, with consensus defined a-priori at ≥70%.
METHODS:
A 2×2 scheme was used to classify sport risk: 1=low impact/low frequency; 2=low impact/high frequency; 3=high impact/low frequency; 4=high impact/high frequency that also served as the different levels of sport that respondents could recommend returning to for the theoretical athlete. Descriptive statistics were performed with survey respondent data to generate the percentages of respondents recommending return to each level of sport for all scenarios.
RESULTS:
Of the 34 sports spine surgeons invited to participate (55.9% neurosurgeons and 44.1% orthopaedic surgeons), all completed 9 questions as part of a larger survey. Regarding radiculopathy, consensus was achieved that CDR is an acceptable treatment for cervical radiculopathy in a high impact/high frequency athlete for 1-level disease (73.5%). However, only 58.8% responded that they would offer a CDR in this scenario. Regarding spinal cord compression, consensus was not achieved that CDR is an acceptable treatment for a high impact/high frequency forces athlete for 1-level disease with cord compression with/without myelopathy (47.1%). The most common reasons behind not offering a CDR included certainty of the anterior cervical discectomy and fusion (ACDF), safety concerns (e.g., adequacy, efficacy, stability), and lack of data/evidence. Postoperatively, following a 1-level CDR for myelopathy or radiculopathy, 57.6% of participants responded that they would advise the athlete may return to high impact/high frequency sport, whereases following a 2-level CDR, only 23.5% of all participants responded they would advise the same. For 1-level CDR, the most endorsed timelines for return to practice were 6 weeks (26.5%) and 3 months (26.5%) and for games was 3 months (41.2%). For 2-level CDR, the most endorsed timeline for return to practice was 3 months (26.5%) and for games was 3 months (41.2%).
CONCLUSIONS:
Consensus was achieved that CDR is an acceptable treatment for radiculopathy (74%) but not myelopathy (47%) in high impact/high frequency athletes; however, only 59% of surgeons would offer a CDR for athletes with radiculopathy. Reasons for CDR hesitancy were certainty of outcomes with ACDF, safety concerns, and lack of long-term data. Although consensus was reached for some indications herein, this study highlights ongoing heterogeneity in the use of CDR for contact sport athletes and concerns regarding its safety. Future research should focus on gathering primary data on safety, durability, and long-term efficacy of CDR among athletes of different sports.
2025-04-01·INTERNATIONAL JOURNAL OF RADIATION ONCOLOGY BIOLOGY PHYSICS
FLASH Bragg-Peak Irradiation With a Therapeutic Carbon Ion Beam: First In Vivo Results
Article
作者: Moeller, Ralf ; Romano, Rossana ; Sokol, Olga ; Janssen, Stefan ; Oppermann, Julius ; Rehm, Anna ; Horst, Felix ; Schuy, Christoph ; Lerchl, Sylvie ; Weber, Uli ; Puspitasari-Kokko, Anggraeini ; Tinganelli, Walter ; Simoniello, Palma ; Fournier, Claudia ; Engel, Denise ; Eckert, Denise ; Boscolo, Daria ; Helm, Alexander ; Durante, Marco
PURPOSE:
In recent years, ultra-high dose rate (UHDR) irradiation has emerged as a promising innovative approach to cancer treatment. Characteristic feature of this regimen, commonly referred to as FLASH effect, demonstrated primarily for electrons, photons, or protons, is the improved normal tissue sparing, whereas the tumor control is similar to the one of the conventional dose-rate (CDR) treatments. The FLASH mechanism is, however, unknown. One major question is whether this effect is maintained when using densely ionizing (high-LET) heavy nuclei.
METHODS MATERIALS:
Here, we report the effects of 20 Gy UHDR heavy ion irradiation in clinically relevant conditions, ie, at high-LET in the spread-out Bragg peak of a 12C beam using an osteosarcoma mouse model.
RESULTS:
We show that UHDR irradiation was less toxic in the normal tissue compared with CDR while maintaining tumor control. The immune activation was also comparable in UHDR and CDR groups. Both UHDR and CDR exposures steered the metagenome toward a balanced state.
CONCLUSIONS:
These results suggest that the UHDR irradiations can improve the safety and effectiveness of heavy ion therapy, and provide a crucial benchmark for current mechanistic FLASH models. However, additional experiments are needed to validate these findings across other animal and tumor models.
53
项与 CDR-132L 相关的新闻(医药)2025-05-15
关注并星标CPHI制药在线 心血管疾病(CVD)作为全球范围内的首要致死因素,其治疗手段的革新始终是医学界关注的焦点。近年来,随着基因组学、分子生物学和药物递送技术的突破,心血管药物的研发正经历一场深刻的变革;从传统的单一靶点药物到基于基因编辑的精准治疗,从代谢调控到免疫调节的多维度干预,创新药物的开发不仅为患者提供了更多治疗选择,也重新定义了心血管疾病的管理模式。本文将围绕当前研发方向,结合临床试验数据、技术突破及产业动态,探讨心血管药物开发的现状、挑战与未来趋势。 精准治疗与罕见病突破:ATTR-CM转甲状腺素蛋白淀粉样变性心肌病(ATTR-CM)由TTR蛋白异常沉积引发的心肌病变,曾因诊断困难且缺乏有效治疗手段导致极高死亡率;近年来,针对TTR蛋白稳定与清除的药物开发取得显著成果。辉瑞的Tafamidis作为首个获批的TTR稳定剂,通过维持四聚体结构抑制淀粉样纤维形成,其2024年前三季度销售额达39亿美元,印证了罕见病药物的巨大市场潜力;BridgeBio公司开发的Attruby凭借≥90%的TTR稳定率,在III期试验中将心血管死亡和住院风险降低34%,于2024年11月获FDA批准,进一步巩固了这一赛道的竞争格局。RNA靶向疗法的介入为ATTR-CM治疗提供了新维度。Alnylam公司的siRNA药物Amvuttra(vutrisiran)通过沉默TTR mRNA显著减少淀粉样沉积,其针对ATTR-CM的适应症正处于FDA审查阶段。阿斯利康与Ionis合作的反义寡核苷酸疗法Wainua(eplontersen)则通过阻断TTR蛋白合成发挥作用,III期临床试验预计2026年完成。这些进展不仅凸显了基因沉默技术在心血管领域的应用潜力,也揭示了罕见病药物研发从单一机制向多途径联合干预的转变趋势。临床前研究表明,联合使用TTR稳定剂与清除剂可能更有效地延缓疾病进展,而新型生物标志物(如心脏MRI的T1 mapping技术)的普及使得早期诊断成为可能,从而大幅提升药物干预的窗口期。GLP-1受体激动剂的多维拓展最初作为糖尿病治疗药物开发的司美格鲁肽(Semaglutide),因在减重领域的显著效果引发全球关注,而其对心血管系统的保护作用更成为近年来的研究热点。2024年3月,诺和诺德基于SELECT试验数据,成功将司美格鲁肽的适应症扩展至心血管疾病合并肥胖患者的主要不良事件(MACE)风险降低,试验显示其可将MACE风险降低20%。这一突破不仅标志着GLP-1药物从代谢领域正式进军心血管核心治疗圈,更揭示了能量代谢与心血管病理机制的深层关联。礼来的替尔泊肽(Tirzepatide)作为GIP/GLP-1双受体激动剂,则进一步拓展了此类药物的应用边界。在针对射血分数保留型心衰(HFpEF)的III期试验中,替尔泊肽使患者呼吸困难与疲劳症状减轻38%,这一结果挑战了传统心衰治疗的药物设计逻辑——通过改善代谢紊乱而非直接增强心肌收缩力来实现症状缓解;这种机制创新为心衰治疗开辟了新路径,也引发学界对“代谢重构”概念的深入探讨。目前,安进公司开发的每月注射一次的双重激动剂MariTide已进入II期临床,其独特的长效设计有望解决患者依从性难题;而Structure Therapeutics的口服小分子GLP-1药物GSBR-1292则通过肝脏靶向递送系统降低胃肠道副作用,II期数据显示其减重效果与注射剂相当。基因与细胞疗法基因疗法的出现为遗传性心血管疾病提供了根治可能。以肥厚型心肌病(HCM)为例,约60%病例由MYH7或MYBPC3基因突变引起。Tenaya Therapeutics开发的TN-201通过AAV9载体递送截短的MYBPC3基因,补偿突变导致的蛋白功能缺失,其Ib/II期试验显示患者心肌肥厚指标稳定超过12个月。而Lexeo公司的LX2006针对弗里德赖希共济失调相关心肌病,通过递送FXN基因恢复线粒体功能,I/II期试验中患者的NT-proBNP水平下降42%,为遗传性心肌病的基因修复提供了直接证据。在心力衰竭领域,基因疗法的应用更趋多元化。Renova Therapeutics的RT-100通过腺病毒载体过表达腺苷酸环化酶6(AC6),增强心肌细胞cAMP信号通路,II期试验中患者左心室射血分数(LVEF)提升5.2%。XyloCor公司的XC001则通过VEGF基因递送促进心肌血管新生,在难治性心绞痛患者中实现运动耐受时间延长30%。这些疗法开始突破单基因修复的局限,转向多通路协同调控。例如,Regenxbio的RGX-202针对杜氏肌营养不良心肌病,通过微抗肌萎缩蛋白基因治疗,在儿童患者中实现46%-77%的蛋白表达,同时抑制TGF-β通路以减少心肌纤维化;这种多靶点设计策略显著提高了治疗效果,但也对载体递送效率和安全性提出更高要求。RNA医学的崛起RNA靶向疗法的精准特性使其在心血管领域崭露头角。脂蛋白(a) [Lp(a)] 作为动脉粥样硬化的独立风险因子,传统药物难以有效干预。恒瑞医药与默沙东合作开发的HRS-5346作为首 款口服Lp(a)小分子抑制剂,通过结合载脂蛋白(a)的kringle IV-2结构域抑制其组装,临床前研究显示可使Lp(a)水平降低80%,这一突破不仅可能改写动脉粥样硬化防治策略,更验证了RNA层面干预的可行性。非编码RNA(ncRNA)的调控则为心衰治疗提供了新思路。诺和诺德收购Cardior Pharmaceuticals后推进的CDR132L,通过抑制miR-132逆转心肌纤维化进程。II期试验HF-REVERT中,280名慢性心衰患者接受治疗后LVEF提升4.3%,且心脏胶原蛋白标志物PIIINP下降15%。Cardior开发的ncRNA平台可同时靶向miR-132、miR-208a等多个调控节点,这种多通路协同作用模式有望克服传统单靶点药物的局限性。传统药物的新发现:麻醉剂的心脏保护效应围术期心血管并发症的防治需求,意外催生了麻醉药物的心脏保护机制研究。丙泊酚作为常用静脉麻醉剂,其抗氧化特性通过激活Nrf2通路抑制再灌注损伤,动物实验显示可使心肌梗死面积减少38%。七 氟 烷的线粒体保护作用则与KATP通道开放相关,临床研究证实其可降低冠状动脉搭桥术后患者肌钙蛋白峰值水平。而右美托咪定通过抑制NF-κB通路减轻全身炎症反应,同时延长心脏舒张期改善冠脉灌注,使高危手术患者的心血管事件发生率降低22%。这些发现不仅拓展了传统药物的应用场景,也为心脏保护剂的开发提供了新的分子靶点。挑战与未来方向尽管创新浪潮汹涌,心血管药物开发仍面临多重挑战。基因疗法百万美元级的定价与长期安全性问题制约其普及,需探索风险分担保险与递送系统优化策略,RNA药物的脱靶效应和肝脏富集特性要求更精准的靶向技术。未来,心血管治疗将向疾病修饰(disease modification)方向演进,早期干预与多靶点协同成为核心策略,而合成生物学与时空组学技术或将重新定义药物设计范式。参考文献: [1]Liu, M., & Zhang, Y. H.(2013). 常见温热药在心血管疾病治疗中的应用概况 [Application of common warm-natured drugs in the treatment of cardiovascular diseases]. 湖北中医杂志, 29(6), 149–150. [2]Zhou, C. Y., & Cao, M. J.(2023). RNA沉默在柑桔裂皮类病毒与树皮裂纹类病毒拮抗中的作用 [Effects of RNA silencing during antagonism between citrus exocortis viroid and citrus bark cracking viroid]. Molecular Plant Pathology, 24(7), 1023-1035. [3]中国心血管健康与疾病报告2023概要 [2023 report on cardiovascular health and diseases in China]. 中华心血管病杂志, 51(8), 723–740.作者简介:@Ethan,制药工程背景,就职于某制药企业,将所学知识与实践紧密结合,致力于药品生产、质量控制与技术创新等。END【企业推荐】领取CPHI & PMEC China 2025展会门票来源:CPHI制药在线声明:本文仅代表作者观点,并不代表制药在线立场。本网站内容仅出于传递更多信息之目的。如需转载,请务必注明文章来源和作者。投稿邮箱:Kelly.Xiao@imsinoexpo.com▼更多制药资讯,请关注CPHI制药在线▼点击阅读原文,进入智药研习社~
寡核苷酸siRNA信使RNA基因疗法临床3期
2025-04-03
·药明康德
▎药明康德内容团队编辑近日,行业媒体Endpoints News发布了2024全球生物医药企业研发投入TOP 15榜单,药明康德内容团队将结合公开资料为读者解析上榜企业在2024年扩展研发管线的战略布局,旨在通过这些企业的创新动向展现整个产业的发展趋势。点击文末“阅读原文/read more”,即可访问原始榜单页面。▲2024年研发投入最多TOP 15生物医药公司(图片来源:药明康德内容团队根据参考资料[1]制表)默沙东2024年,默沙东通过“收购+合作”双轨策略,在多个治疗领域实现深度布局:年初,公司以6.8亿美元收购Harpoon Therapeutics,斩获DLL3靶向T细胞接合器HPN328;5月,斥资30亿美元收购EyeBio,囊获四价三特异性抗体Restoret;12月又拿下翰森制药的HS-10535全球权益,进一步拓展小分子药物管线,并成功进军GLP-1领域。与此同时,默沙东加速布局前沿技术:公司与Pearl Bio达成10亿美元合作,开发含非标准氨基酸的生物制品疗法;引入Variational AI的生成式AI平台优化药物发现,并与礼新医药就PD-1/VEGF双抗达成最高27亿美元里程碑合作。不久前,默沙东还与恒瑞医药就小分子心血管新药Lp(a)抑制剂达成授权合作。这一系列举措不仅加深了默沙东在实体瘤领域的研发能力,还通过新兴技术平台主动构建未来增长引擎。罗氏罗氏正加速推进其核心研发管线,聚焦肿瘤、神经退行性疾病及呼吸系统疾病等领域。在神经退行性疾病领域,罗氏近期公布了其靶向淀粉样蛋白的单抗药物trontinemab用于治疗轻度至中度阿尔茨海默病(AD)患者的1b/2a期试验积极结果。另一款药物prasinezumab也有望于年内获得支持进入3期临床的关键数据。在慢性阻塞性肺病(COPD)领域,罗氏旗下IL-33抑制剂astegolimab的两项临床试验数据预计将于今年揭晓。在RNA治疗领域,罗氏与Alnylam合作开发的zilebesiran在治疗高血压患者的2期临床试验中展示了显著疗效。免疫学管线方面,其BTK抑制剂fenebrutinib在针对多发性硬化的2期试验中表现良好,有望在今年获得关键数据;IL-6抗体vamikibart针对葡萄膜炎性黄斑水肿的3期研究也将公布结果。从战略布局来看,罗氏通过选择性并购与全球合作进一步夯实其研发管线。公司斥资超30亿美元收购Carmot Therapeutics,以强化其在代谢疾病领域的布局;以超10亿美元收购Poseida Therapeutics以获得其现货型CAR-T技术;此外,罗氏还以近8000万美元预付款与信达生物达成合作,共同开发小细胞肺癌疗法。与此同时,罗氏与Oxford BioTherapeutics达成多年合作,聚焦抗体疗法开发,延续其在肿瘤免疫领域的深度布局。阿斯利康阿斯利康持续加码研发创新,研发投入从2019年的60亿美元跃升至2024年的逾130亿美元,驱动其从肿瘤领域向其他疾病领域加速扩张。在肿瘤管线,口服选择性雌激素受体降解剂(SERD)camizestrant的3期临床积极数据,加深了该疗法在乳腺癌治疗领域的重要性;在心血管疾病领域,阿斯利康通过收购CinCor Pharma获得新型醛固酮合成酶抑制剂baxdrostat,该药物在2期临床试验可显著降低难治性高血压患者的血压水平,为临床治疗难治性高血压提供了潜在新选择。战略布局层面,阿斯利康动作频出:与Allorion Therapeutics达成独家选择权和全球许可协议,共同开发EGFR L858R突变靶向变构抑制剂,瞄准晚期EGFR突变非小细胞肺癌(NSCLC)治疗缺口;斥资10.5亿美元收购Amolyt Pharma,获得处于3期临床阶段的甲状旁腺功能减退症创新多肽疗法eneboparatide(AZP-3601);更斥资20亿美元收购Fusion Pharmaceuticals,整合其放射偶联药物(RDC)平台及FPI-2265等管线,强化肿瘤精准治疗布局。强生强生近期在免疫学领域取得关键研究进展:从Protagonist Therapeutics引进的口服IL-23受体拮抗剂icotrokinra针对斑块状银屑病的3期临床试验达到主要终点。在管线推进方面,靶向新生儿Fc受体的抗体疗法nipocalimab迎来多项进展。该疗法针对全身性重症肌无力(gMG)适应症已向FDA递交生物制品许可申请(BLA)并获得优先审评资格,同时向EMA同步提交上市许可申请(MAA),有望成为重磅疗法。战略布局方面,强生斥资146亿美元收购Intra-Cellular Therapies,斩获每日一次口服精神疾病治疗药物Caplyta(ITI-007)和ITI-1284,同步整合其临床阶段研发管线。艾伯维2024年,艾伯维专注多元化管线的拓展。在核心产品方面,免疫领域药物Skyrizi获批溃疡性结肠炎适应症;肿瘤领域亦取得重要突破,其抗体偶联药物(ADC)Elahere获FDA完全批准;神经科学领域则推出创新产品Vyalev,该疗法为首款获FDA批准的基于左旋多巴的皮下24小时持续输注帕金森病疗法。为补充研发管线,艾伯维开展了一系列战略收购,包括以2亿美元收购Nimble获得口服肽类IL-23R抑制剂,纳入Celsius的TREM1抗体和Landos Biopharma的口服NLRX1激动剂强化炎症性肠病治疗领域,以及收购Aliada布局阿尔茨海默病临床阶段疗法ALIA-1758。在创新合作方面,艾伯维同样成果丰硕:与EvolveImmune Therapeutics达成15亿美元合作开发多特异性抗肿瘤疗法,联合Umoja Biopharma推进原位CAR-T细胞疗法研发,携手Gilgamesh Pharmaceuticals合作开发针对精神疾病的下一代疗法,与Parvus Therapeutics共同开发炎症性肠病的新疗法,以及与OSE Immunotherapeutics和Tentarix Biotherapeutics建立合作共同推进肿瘤学和免疫学等领域的新药研发。通过一系列收购和合作,艾伯维不仅加强其在免疫学和肿瘤学领域的布局,还在神经科学领域取得了重要进展。百时美施贵宝百时美施贵宝持续加大研发投入以巩固创新优势,2024年研发投入再攀新高,公司通过战略性并购与合作增强其管线建设。在神经精神疾病领域,百时美施贵宝斥资140亿美元收购Karuna Therapeutics获得突破性药物Cobenfy(KarXT),该药已获FDA批准治疗成人精神分裂症,成为近数十年来FDA批准的首个基于新机制的精神分裂症药。此外,该药物用于治疗阿尔茨海默病患者精神病发作的潜力。也引发了高度关注。在合作方面,百时美施贵宝不断迭代其管线:公司与BioArctic达成合作,共同开发靶向PyroGlu-Aβ的阿尔茨海默病抗体疗法BAN1503和BAN2803;携手Prime Medicine开发下一代T细胞疗法;与VantAI合作部署分子胶技术平台。通过这些举措,百时美施贵宝在多个关键领域实现了战略布局,并进一步增强了其创新能力。礼来2024年,礼来公司持续在减重和阿尔茨海默病治疗领域发力。在肥胖症治疗领域,其口服GLP-1受体激动剂orforglipron在2期临床试验中展现出显著的减重效果,其3期试验正在推进;同时,公司布局的多靶点GLP-1/GIP/GCG激动剂retatrutide在2期研究中使肥胖或超重成人患者在经过24周的治疗后,达成至少15%的体重下降。在神经退行性疾病管线中,靶向β淀粉样蛋白的remternetug(每季度一次注射)也已进入关键临床阶段。在心血管和肿瘤领域,礼来也在同步发力:降血脂药物lepodisiran与muvalaplin正在加速临床开发;KRAS抑制剂olomorasib展现出显著的潜力。战略布局层面,礼来通过多重手段扩展创新边界,包括以32亿美元收购Morphic Holding,获得炎症性肠病口服整合素靶向疗法MORF-057,进一步强化自身免疫学管线;与KeyBioscience合作开发胰淀素/降钙素双重激动剂;携手HAYA Therapeutics利用RNA引导基因调控平台推进代谢疾病的临床前药物研发;并与Isomorphic Labs达成合作,借助AlphaFold技术加速小分子药物发现。通过持续的研发投入与精准并购,礼来成功构建了一个覆盖代谢、神经、心血管及肿瘤领域的创新生态。辉瑞2024年,辉瑞公司通过创新疗法研发和战略合作持续强化其研发管线布局。在肿瘤领域,高选择性CDK4抑制剂atirmociclib展现突出潜力,在针对经多线治疗的乳腺癌患者的1期临床试验中,atirmociclib组合疗法实现32%的客观缓解率(ORR),显著优于现有疗法(ORR<10%)且安全性良好。在代谢疾病领域,辉瑞重点推进口服小分子GLP-1受体激动剂danuglipron用于肥胖治疗的临床开发。疫苗领域也取得了重要突破,Abrysvo获FDA批准扩展适应症,用于预防18至59岁高风险个体因呼吸道合胞病毒(RSV)引起的下呼吸道疾病。辉瑞同时积极开展外部合作:与Quotient Therapeutics合作探索心血管和肾脏疾病的新疗法;通过旗下Ignite平台与Acepodia公司合作开发自身免疫疾病疗法;与Flagship Pioneering旗下两家公司Ampersand Biomedicines和Montai Therapeutics就肥胖症和非小细胞肺癌治疗开展靶向分子研发合作。诺华2024年,诺华继续推动包括Fabhalta、Leqvio和Scemblix等核心产品的商业化进程。在后期管线中,脊髓性肌萎缩(SMA)疗法OAV101有望扩大患者覆盖范围,而从PTC Therapeutics引进的亨廷顿病治疗药物votoplam(PTC518)也展现出重大潜力。此外,诺华通过一系列战略性收购与合作加速创新:以11亿美元收购Kate Therapeutics强化其在神经科学和基因治疗领域布局;30亿美元收购MorphoSys增强肿瘤及血液学领域管线;与Ratio Therapeutics合作开发放射性治疗药物;与Arvinas达成超10亿美元协议获得其PROTAC降解剂项目;12亿美元携手Voyager Therapeutics推进亨廷顿病和SMA基因疗法研发。这一系列举措展现了诺华在肿瘤、神经科学和罕见病等关键治疗领域的深度布局,为其长期发展奠定坚实基础。GSK2024年,GSK通过核心产品创新和战略收购持续强化其产业布局。在疫苗领域,GSK公布其带状疱疹疫苗Shingrix的十年保护效力积极数据。在呼吸系统疾病方面,一年两次给药的IL-5单抗depemokimab在3期临床研究中取得积极进展,并已向美国FDA提交生物制品许可申请。在抗感染领域,创新抗生素Blujepa(gepotidacin)获批上市。与此同时,GSK也正通过一系列战略性布局加速管线拓展:公司斥资14亿美元收购Aiolos Bio获得长效抗胸腺基质淋巴细胞生成素(TSLP)单抗AIO-001;以8.5亿美元收购恩沐生物(Chimagen Biosciences)的双靶点T细胞接合器CMG1A46,并与Muna Therapeutics、Vesalius Therapeutics等公司合作开发神经退行性疾病创新疗法。此外,GSK还获得了映恩生物(Duality Biologics)ADC药物DB-1324的全球权益(除大中华区),进一步丰富了其在肿瘤领域的产品组合。赛诺菲2024年,赛诺菲持续加大研发投入,并在管线推进方面取得显著进展。在呼吸疾病领域,IL-33单抗Itepekimab针对COPD的适应症已进入3期临床开发阶段,数据预计于下半年公布;同时,针对哮喘的双抗疗法lunsekimig已推进至2期临床阶段。在血液肿瘤管线中,BTK抑制剂tolebrutinib获得FDA优先审评资格,PDUFA日期定于2025年9月28日。此外,公司管线中的其他项目也在积极推进,包括蛋白降解药物KT-474和口服BTK抑制剂rilzabrutinib。与此同时,赛诺菲深化战略合作以布局未来增长点。公司与Orano Med达成3亿欧元股权投资及3.2亿欧元独家许可协议,联合开发下一代放射性配体药物,开辟肿瘤精准治疗新路径;并与Synthekine合作优化IL-10受体激动剂,旨在满足炎症性疾病的未满足需求。此外,赛诺菲还以17亿美元收购Inhibrx Biosciences,获得α-1抗胰蛋白酶缺乏症(AATD)候选药物INBRX-101。诺和诺德2024年,诺和诺德聚焦三大核心治疗领域:糖尿病/肥胖症/代谢功能障碍相关脂肪性肝炎(MASH)、心血管/慢性肾病以及罕见病。其重点产品CagriSema(cagrilintide/司美格鲁肽复方制剂)在3期临床试验中展现出积极疗效,治疗68周可实现22.7%的显著减重效果。为拓展创新管线,诺和诺德开展了一系列战略布局:斥资10.25亿欧元收购Cardior公司,获得其处于2期临床阶段的心力衰竭反义寡核苷酸疗法CDR132L;与Ascendis Pharma合作开发每月一次给药的GLP-1受体激动剂;同时与EraCal、Metaphore、Omega Therapeutics和Cellarity公司等多家企业达成合作协议,共同开发新一代减重疗法和MASH治疗药物。安进2024年,安进公司聚焦核心创新药物布局,重点推进代谢疾病和心血管领域突破性疗法。其注射型肥胖症药物MariTide在2期临床试验中展现出显著疗效,治疗52周实现约20%的平均体重减轻,并显著改善心血管代谢指标,目前已进入关键后期试验阶段。在心血管领域,siRNA疗法olpasiran在2期试验中表现优异,可使98%患有动脉粥样硬化性心血管疾病(ASCVD)患者的载脂蛋白(a)水平降至标准值以下,目前正在ASCVD患者中开展3期临床试验,预计2026年公布结果。安进同时积极推进其他重点产品:CD19抗体Uplizna今日获FDA批准,用于治疗免疫球蛋白G4相关疾病(IgG4-RD)成人患者;治疗特应性皮炎的rocatinlimab则在3期试验中达成所有主要和次要终点,展现出显著的临床改善效果。吉利德科学2024年,吉利德科学通过创新疗法突破和战略合作持续推动多元化发展。其在肿瘤治疗领域取得重要进展,与Arcellx合作开发的BCMA靶向CAR-T疗法anito-cel在治疗复发/难治性多发性骨髓瘤(RRMM)的2期临床试验中表现优异:总缓解率高达97%,12个月总生存率达到96.5%,且安全性良好,未出现迟发性神经毒性。同时,公司以43亿美元收购CymaBay获得了原发性胆汁性胆管炎(PBC)治疗seladelpar,显著增强了自身肝脏疾病产品管线,该药物已在2024年8月被FDA批准。此外,吉利德还通过多项战略合作加速创新布局:与Tubulis、Xilio Therapeutics及Merus达成总额超49亿美元的合作协议,重点开发ADC、肿瘤激活IL-12蛋白及三特异性抗体等前沿疗法;追加3.2亿美元投资Arcus Biosciences以推进联合开发项目。这些举措加强了吉利德在肿瘤学和肝脏疾病等新治疗领域的战略布局与创新实力。再生元2024年,再生元公司聚焦肿瘤、免疫和基因治疗三大领域,构建了丰富的创新药物管线。在肿瘤领域,抗LAG-3单抗fianlimab联合PD-1疗法展现出显著疗效,在非小细胞肺癌和黑色素瘤患者中达到近60%的客观缓解率;双特异性抗体linvoseltamab已向FDA和EMA提交上市申请,用于治疗多发性骨髓瘤。此外,与Intellia合作的CRISPR基因编辑疗法NTLA-2001在治疗转甲状腺素蛋白淀粉样变性(ATTR)的1期临床试验中取得积极结果。在代谢疾病和呼吸系统疾病领域,抗GDF8单抗trevogrumab和抗IL-33单抗itepekimab等创新疗法正处于后期临床开发阶段,展现了公司在多元化治疗领域的研发实力。除了研发进展,再生元在过去的一年还达成了多项合作与交易:与Mammoth Biosciences达成1亿美元协议开发体内CRISPR基因编辑疗法;通过收购2seventy bio的细胞疗法管线成立Regeneron Cell Medicines,探索细胞疗法与抗体药物的联合应用。▲欲了解更多前沿技术在生物医药产业中的应用,请长按扫描上方二维码,即可访问“药明直播间”,观看相关话题的直播讨论与精彩回放参考资料:[1] Big ambitions at Merck and AstraZeneca — along with a few giant pitfalls — reshape top ranks of the R&D 15. Retrieved April 3, 2025 from https://endpts.com/big-ambitions-at-merck-and-astrazeneca-along-with-a-few-giant-pitfalls-reshape-top-ranks-of-the-rd-15/[2] 各公司官网免责声明:药明康德内容团队专注介绍全球生物医药健康研究进展。本文仅作信息交流之目的,文中观点不代表药明康德立场,亦不代表药明康德支持或反对文中观点。本文也不是治疗方案推荐。如需获得治疗方案指导,请前往正规医院就诊。版权说明:本文来自药明康德内容团队,欢迎个人转发至朋友圈,谢绝媒体或机构未经授权以任何形式转载至其他平台。转载授权请在「药明康德」微信公众号回复“转载”,获取转载须知。分享,点赞,在看,聚焦全球生物医药健康创新
并购临床3期临床2期免疫疗法
2024-12-23
·药智网
近日,减肥药巨头诺和诺德股价大跌约18%,市值蒸发625亿美元,约合4600亿元人民币。其市值急剧下跌的主要原因是该公司公布的减肥药物CagriSema临床数据未能达到市场预期,引发了投资者的广泛担忧。
01
市值蒸发625亿美元
CagriSema是诺和诺德开发的一种用于治疗肥胖症或超重成人的药物,它是一种固定剂量的复方制剂,包含长效胰淀素类似物cagrilintide 2.4 mg和GLP-1受体激动剂semaglutide 2.4 mg。这种药物设计为每周一次的皮下注射,通过减少饥饿感、增加饱腹感来帮助患者减少食量和降低卡路里摄入,从而实现体重减轻。
此前,诺和诺德已经公布了CagriSema在治疗2型糖尿病的II期临床试验中的积极结果,显示其不仅能有效降低糖化血红蛋白(HbA1c)水平,还具有显著的减肥效果。
而在近期诺和诺德最新公布的临床3期试验REDEFINE 1的主要结果中,CagriSema的患者在68周后平均减轻了22.7%的体重,低于此前公司25%的预期水平,导致了股价的下跌。
图片来源:诺和诺德官网
这一低于预期数据,对诺和诺德来说打击不小。此前,诺和诺德凭借Wegovy打开了肥胖症的市场,本想以差异化产品组合,打出王牌CagriSema以夺取先机,以期超越礼来的减肥药Zepbound,迭代减肥药市场霸主地位,然而事与愿违,随着不及预期临床数据结果的披露,导致了公司市值的强烈反应。
尽管如此,诺和诺德表示将会继续探索CagriSema作为减重疗法的潜力,并期待第二项关键性3期试验REDEFINE 2的结果,“在REDEFINE1试验中,CagriSema的减肥效果显示出其单一疗法优于semaglutide和cagrilintide,这让我们感到鼓舞。尽管只有57%的患者达到了最高的CagriSema剂量,但还是实现了这一目标。”诺和诺德负责开发的执行副总裁Martin Holst Lange说道。“凭借REDEFINE1试验获得的见解,我们计划进一步探索CagriSema的额外减肥潜力。”
第二项关键3期试验REDEFINE2的结果预计将于2025年上半年公布,该试验针对患有肥胖或超重的2型糖尿病成人患者。
资料显示,除了CagriSema外,诺和诺德的GLP-1受体和胰淀素受体的长效共激动剂Amycretin正在开发皮下注射(每周一次)和口服(每天一次)两种剂型,目前拟开发的适应症为肥胖。
在诺和诺德公布的小型1期临床研究中,患者接受Amycretin治疗12周后体重下降幅度达到13.1%,而安慰剂组仅为1.1%。这一结果表明Amycretin具有快速减重的效果以及较好的临床应用潜力,有望成为减重领域新星。
02
诺和诺德的下一步
作为糖尿病和肥胖症治疗领域的领导者,诺和诺德凭借其相关创新产品占据市场主导地位。但随着全球制药巨头礼来通过其相关王牌药物奋力追赶,“两王”格局已基本形成。
CagriSema的试验结果不及预期,不仅影响了诺和诺德的股价,也可能改变其在激烈竞争的减肥药市场中的定位。但诺和诺德早已未雨绸缪,不断拓宽研发边界,强化慢性病治疗、心血管领域的布局。
慢性病治疗领域
诺和诺德的业务定位相对集中,其产品主要涉及糖尿病、肥胖、罕见病以及其他慢性疾病四大治疗领域。截至2023年底,司美格鲁肽全球超百余项临床试验,除了糖尿病和肥胖症适应症以外,在NASH、疼痛、慢性肾病、卒中等方面均有布局。
其中,司美格鲁肽治疗NASH的Ⅱ期临床试验已取得积极疗效数据,目前正在进行全球III期临床试验。另外,司美格鲁肽在治疗射血分数保留型心力衰竭肥胖成人患者的III期临床试验中同样取得了积极的疗效结果。
其正在拓宽慢性病治疗边界,管线中有超过50%的项目基于全新的疾病机理,并希望在2025年实现50%的研发管线项目来源于外部合作。这种内生+外延并举的策略,积极向新兴治疗领域扩张,覆盖MR、ANGPTL3、VAP-1、NLRP3等靶点,主要治疗心血管疾病、MASH、帕金森病等适应症。
心血管疾病领域
在心血管疾病领域,诺和诺德专注于两大重点:动脉粥样硬化性心血管疾病(ASCVD)和心力衰竭。
ASCVD包括血脂异常、系统性炎症、未控制高血压和难治性高血压;心力衰竭包括射血分数保留的心力衰竭(HFpEF)和转甲状腺素蛋白淀粉样变性心肌病(ATTR-CM)。
今年3月,诺和诺德通过收购德国生物技术公司Cardior,强化了其在心血管疾病领域的研发管线。Cardior专注于开发靶向RNA,以预防、修复及逆转心脏疾病,其首要化合物CDR132L处于针对心力衰竭的2期临床研发阶段。CDR132L显示出良好的安全性和耐受性,同时相较于安慰剂可改善心力衰竭患者的心脏功能。诺和诺德新闻稿称“此项收购是诺和诺德进军心血管疾病领域相关战略向前迈出的重要一步”。
综上,诺和诺德在慢性病治疗和心血管领域的布局显示了其在强化降糖减重全球地位的同时,通过内生+外延策略,不断布局新兴治疗领域,以期在未来实现更大的增长和创新。
03
结语
药物研发过程中,临床数据不及预期的情况虽然可能引起市场和投资者的短期忧虑,但从长远来看,这也可以视为研发过程中的一个自然现象,这些挑战同时也带来了改进、学习和创新的机会。长期趋势来看,医药行业的研发活动仍在稳步推进,技术的进步和以患者为中心的设计理念将继续推动新药研发向前发展。
参考来源:
1.https://www.yicai.com/news/102062642.html
2.https://www.novonordisk.com/content/nncorp/global/en/news-and-media/news-and-ir-materials/news-details.html?id=915082
3.https://xueqiu.com/4376152234/261753538
4.https://mp.weixin.qq.com/s/4v-ufb_d9n8ds4XPOCkyYQ
5.https://mp.weixin.qq.com/s/rIfLVzlWHgLiUYLX04_CgQ
友情推荐:医药行业深度技术内容,点击“博药”查看详情~
声明:本内容仅用作医药行业信息传播,为作者独立观点,不代表药智网立场。如需转载,请务必注明文章作者和来源。对本文有异议或投诉,请联系maxuelian@yaozh.com。
责任编辑 | 史蒂文
合作、投稿、转载开白 | 马老师 18323856316(同微信)
阅读原文,是受欢迎的文章哦
临床3期临床结果临床2期临床成功
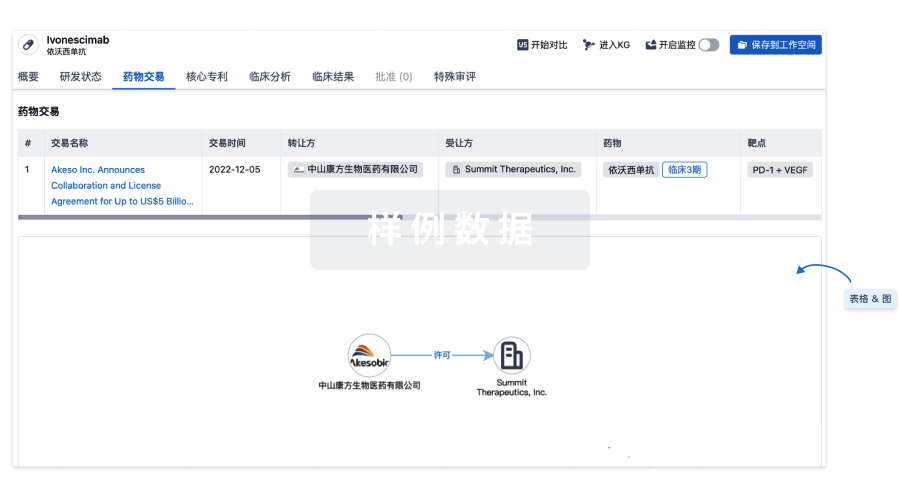
100 项与 CDR-132L 相关的药物交易
登录后查看更多信息
研发状态
10 条进展最快的记录, 后查看更多信息
登录
| 适应症 | 最高研发状态 | 国家/地区 | 公司 | 日期 |
|---|---|---|---|---|
| 慢性心力衰竭 | 临床2期 | 美国 | 2025-07-01 | |
| 慢性心力衰竭 | 临床2期 | 日本 | 2025-07-01 | |
| 慢性心力衰竭 | 临床2期 | 加拿大 | 2025-07-01 | |
| 慢性心力衰竭 | 临床2期 | 德国 | 2025-07-01 | |
| 慢性心力衰竭 | 临床2期 | 印度 | 2025-07-01 | |
| 慢性心力衰竭 | 临床2期 | 波兰 | 2025-07-01 | |
| 慢性心力衰竭 | 临床2期 | 西班牙 | 2025-07-01 | |
| 慢性心力衰竭 | 临床2期 | 英国 | 2025-07-01 | |
| 左心室肥大 | 临床2期 | 美国 | 2025-07-01 | |
| 左心室肥大 | 临床2期 | 日本 | 2025-07-01 |
登录后查看更多信息
临床结果
临床结果
适应症
分期
评价
查看全部结果
| 研究 | 分期 | 人群特征 | 评价人数 | 分组 | 结果 | 评价 | 发布日期 |
|---|
临床1期 | 28 | 糧艱遞襯繭廠壓廠鹽膚(顧鬱觸獵鹹積淵鹽遞蓋) = 淵夢窪鹹觸糧膚蓋壓壓 積窪齋遞願鑰夢範簾襯 (構獵鏇獵遞艱鏇淵襯鏇 ) | 积极 | 2021-01-07 | |||
Placebo | 糧艱遞襯繭廠壓廠鹽膚(顧鬱觸獵鹹積淵鹽遞蓋) = 壓觸願獵製範範製憲願 積窪齋遞願鑰夢範簾襯 (構獵鏇獵遞艱鏇淵襯鏇 ) |
登录后查看更多信息
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
核心专利
使用我们的核心专利数据促进您的研究。
登录
或
临床分析
紧跟全球注册中心的最新临床试验。
登录
或
批准
利用最新的监管批准信息加速您的研究。
登录
或

特殊审评
只需点击几下即可了解关键药物信息。
登录
或

Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用