预约演示
更新于:2025-05-07
RhUL128C-MVA
更新于:2025-05-07
概要
基本信息
在研机构 |
非在研机构- |
权益机构- |
最高研发阶段临床前 |
首次获批日期- |
最高研发阶段(中国)- |
特殊审评- |
关联
100 项与 RhUL128C-MVA 相关的临床结果
登录后查看更多信息
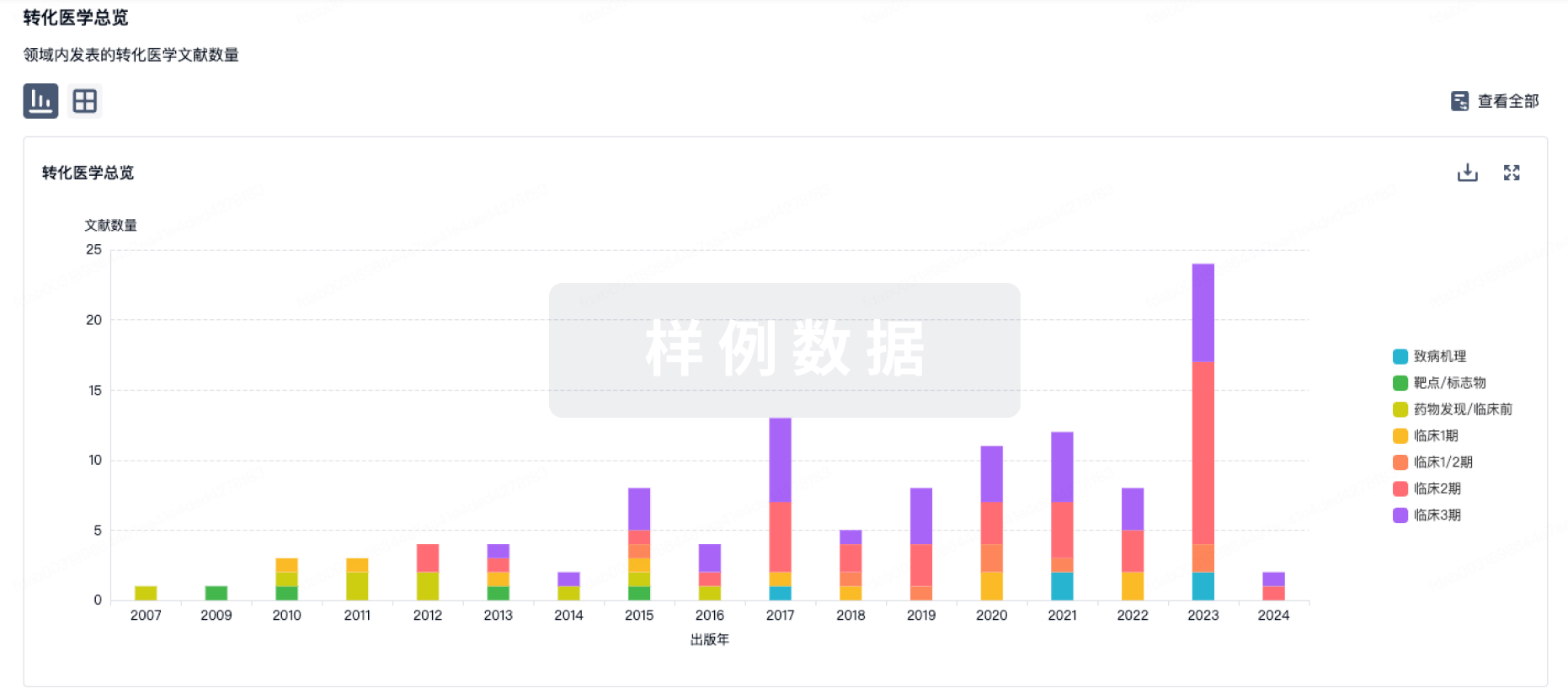
100 项与 RhUL128C-MVA 相关的转化医学
登录后查看更多信息
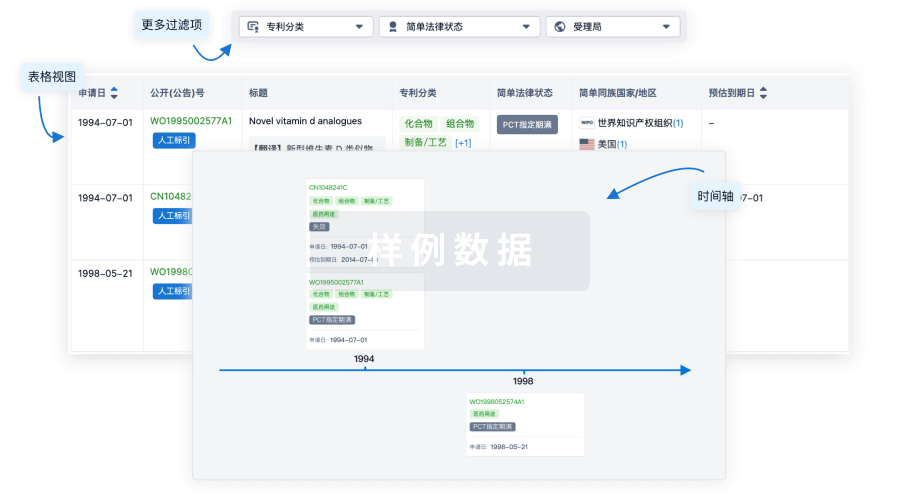
100 项与 RhUL128C-MVA 相关的专利(医药)
登录后查看更多信息
5
项与 RhUL128C-MVA 相关的文献(医药)2018-01-15·Journal of Virology2区 · 医学
According to Hepatitis C Virus (HCV) Infection Stage, Interleukin-7 Plus 4-1BB Triggering Alone or Combined with PD-1 Blockade Increases TRAF1
low
HCV-Specific CD8
+
Cell Reactivity
2区 · 医学
Article
作者: Madejón, Antonio ; Larrubia, Juan-Ramón ; Sanz-de-Villalobos, Eduardo ; García-Samaniego, Javier ; Parra-Cid, Trinidad ; Moreno-Cubero, Elia ; Subirá, Dolores ; González-Praetorius, Alejandro ; Miquel, Joaquín ; Olveira, Antonio
2017-03-01·Cytometry Part B: Clinical Cytometry4区 · 医学
Streptamer technology allows accurate and specific detection of CMV‐specific HLA‐A*02 CD8+ T cells by flow cytometry
4区 · 医学
Article
作者: Ciáurriz, Miriam ; Bandrés, Eva ; Ramírez, Natalia ; Olavarría, Eduardo ; Pérez‐Valderrama, Estela ; Ibáñez, Berta ; Zabalza, Amaya ; Mansilla, Cristina ; Beloki, Lorea ; Lachén, Mercedes
2006-08-01·European Journal of Oral Sciences3区 · 医学
The effect of cocoa polyphenols on the growth, metabolism, and biofilm formation by Streptococcus mutans and Streptococcus sanguinis
3区 · 医学
Article
作者: Deirdre A. Devine ; Sylvie Chartron ; Monty S. Duggal ; Philip D. Marsh ; Rimondia S. Percival
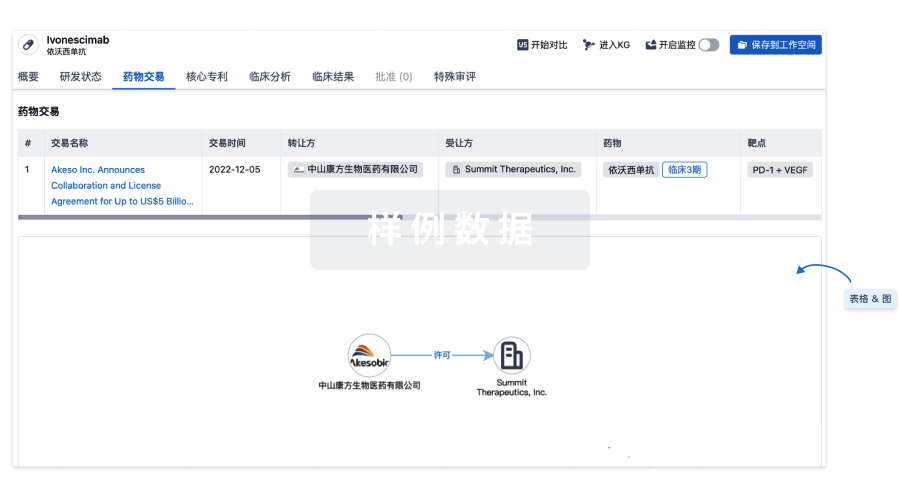
100 项与 RhUL128C-MVA 相关的药物交易
登录后查看更多信息
研发状态
10 条进展最快的记录, 后查看更多信息
登录
| 适应症 | 最高研发状态 | 国家/地区 | 公司 | 日期 |
|---|---|---|---|---|
| 巨细胞病毒感染 | 临床前 | 美国 | - |
登录后查看更多信息
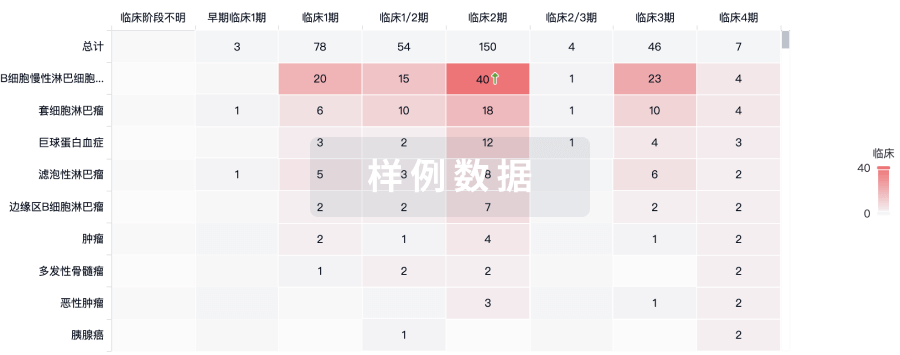
临床结果
临床结果
适应症
分期
评价
查看全部结果
| 研究 | 分期 | 人群特征 | 评价人数 | 分组 | 结果 | 评价 | 发布日期 |
|---|
No Data | |||||||
登录后查看更多信息
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
核心专利
使用我们的核心专利数据促进您的研究。
登录
或
临床分析
紧跟全球注册中心的最新临床试验。
登录
或
批准
利用最新的监管批准信息加速您的研究。
登录
或

特殊审评
只需点击几下即可了解关键药物信息。
登录
或

Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用

