预约演示
更新于:2025-08-06
FS-120
更新于:2025-08-06
概要
基本信息
药物类型 双特异性抗体 |
别名 FS 120 |
作用方式 激动剂 |
作用机制 4-1BB激动剂(肿瘤坏死因子受体超家族成员9激动剂)、OX40激动剂(肿瘤坏死因子受体超家族成员4激动剂) |
治疗领域 |
非在研适应症- |
原研机构 |
非在研机构 |
最高研发阶段临床1期 |
首次获批日期- |
最高研发阶段(中国)- |
特殊审评- |
登录后查看时间轴
关联
1
项与 FS-120 相关的临床试验NCT04648202
A Phase 1/1b Open-Label Study to Evaluate the Safety and Antitumor Activity of FS120, an OX40/CD137 Bispecific Antibody, Alone and in Combination With Pembrolizumab, in Subjects With Advanced Malignancies
This is a Phase 1/1b, multicenter, open label study to evaluate the Safety and Antitumor Activity of FS120, an OX40/CD137 Bispecific Antibody, Alone and in Combination with Pembrolizumab, in Subjects with Advanced Malignancies
开始日期2020-11-18 |
申办/合作机构  invoX Pharma Ltd. invoX Pharma Ltd. [+1] |
100 项与 FS-120 相关的临床结果
登录后查看更多信息
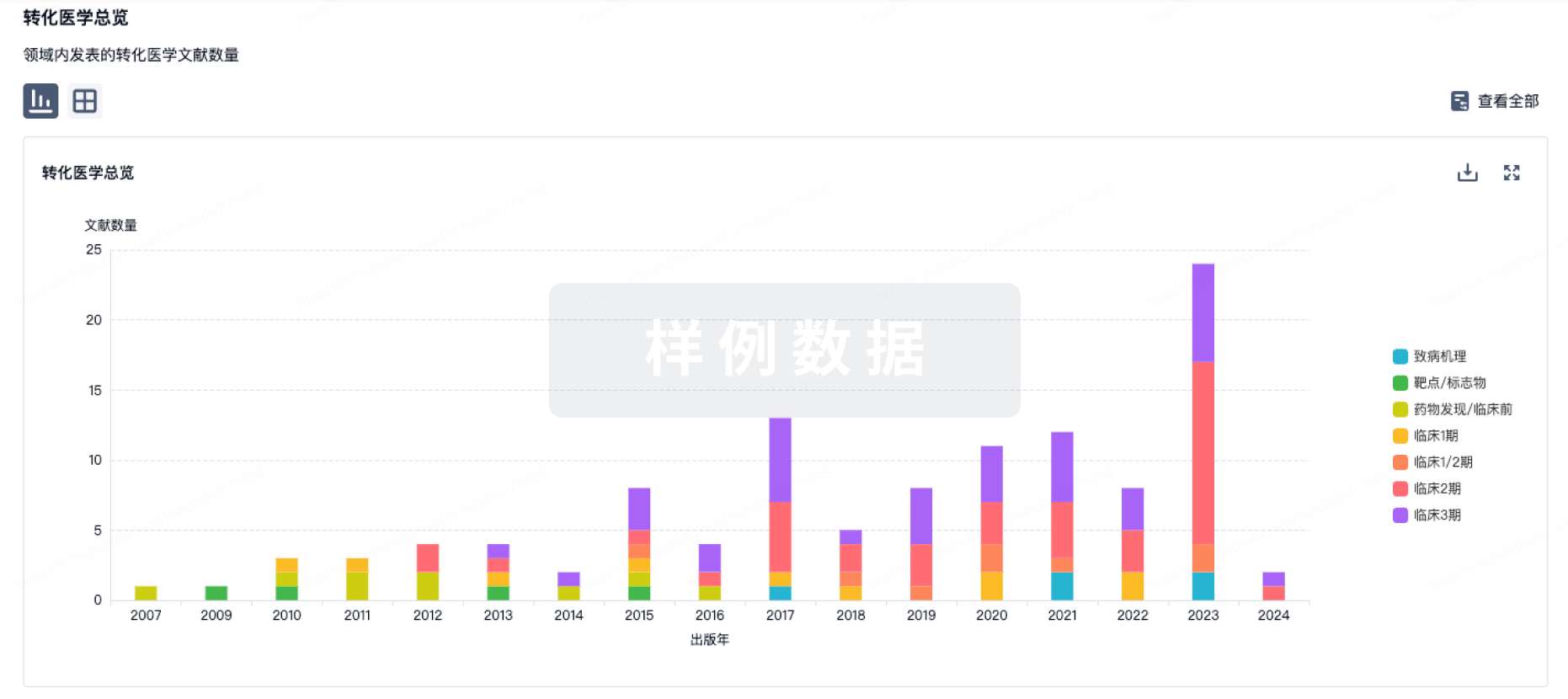
100 项与 FS-120 相关的转化医学
登录后查看更多信息
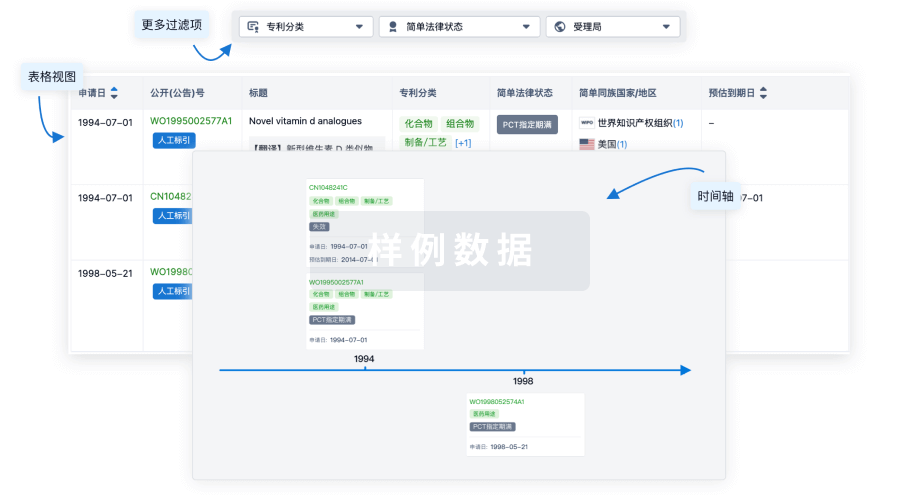
100 项与 FS-120 相关的专利(医药)
登录后查看更多信息
2
项与 FS-120 相关的文献(医药)2020-06-01·Cancer immunology research1区 · 医学
CD137/OX40 Bispecific Antibody Induces Potent Antitumor Activity that Is Dependent on Target Coengagement
1区 · 医学
Article
作者: Everett, Katy L. ; Pravin, John ; Uhlenbroich, Sandra ; Tuna, Mihriban ; Morrow, Michelle ; Wollerton, Francisca ; Brewis, Neil ; Rodrigues, Leonor ; Gaspar, Miguel
Abstract:
Following the success of immune checkpoint blockade therapy against cancer, agonistic antibodies targeting T-cell costimulatory pathways are in clinical trials. The TNF superfamily of receptors (TNFRSF) members CD137 and OX40 are costimulatory receptors that stimulate T-cell proliferation and activation upon interaction with their cognate ligands. Activating CD137 and OX40 with agonistic mAbs stimulates the immune system due to their broad expression on CD4+ and CD8+ T cells and natural killer cells and has antitumor effects in preclinical models. Most TNFRSF agonist antibodies require crosslinking via Fcγ receptors (FcγR), which can limit their clinical activity. FS120 mAb2, a dual agonist bispecific antibody targeting CD137 and OX40, activated both CD4+ and CD8+ T cells in an FcγR-independent mechanism, dependent on concurrent binding. A mouse surrogate version of the bispecific antibody displayed antitumor activity in syngeneic tumor models, independent of T regulatory cell depletion and of FcγR interaction, but associated with peripheral T-cell activation and proliferation. When compared with a crosslink-independent CD137 agonist mAb, the FS120 surrogate induced lower liver T-cell infiltration. These data support initiation of clinical development of FS120, a first-in-class dual agonist bispecific antibody for the treatment of human cancer.
2011-08-01·Annals of vascular surgery4区 · 医学
Use of Fibrin Sealant as a Hemostatic Agent in Expanded Polytetrafluoroethylene Graft Placement Surgery
4区 · 医学
Article
作者: Sandra G. Burks ; Isabella Presch ; Satish Muluk ; Worthington Schenk ; Sibu P. Saha ; Borislava G. Pavlova ; Ani Grigorian ; Bettina Ploder ; Edith Hantak
BACKGROUND:
The low thrombogenicity, porosity, and limited elasticity of expanded polytetrafluoroethylene (ePTFE) vascular grafts, although beneficial, may exacerbate the problem of suture-line bleeding at vascular anastomoses and consequently lead to increased operating times. The overall objective of this prospective, randomized, controlled, subject-blinded, multicenter phase 2 study was to evaluate the efficacy and safety of a fibrin sealant containing 500 IU/mL thrombin and synthetic aprotinin (FS; marketed in the United States under the name TISSEEL) for hemostasis in subjects undergoing vascular surgery and receiving prosthetic ePTFE vascular grafts.
METHODS:
FS was compared with manual compression with surgical gauze pads, a standard of care for hemostasis in vascular surgery. Two FS polymerization/setting times (60 and 120 seconds) were investigated to evaluate influence on the efficacy results. Patients undergoing ePTFE graft placement surgery (N = 73) who experienced bleeding that required treatment after surgical hemostasis were randomized to be treated with FS with clamps opened at 60 seconds (FS-60; N = 26), with FS with clamps opened at 120 seconds (FS-120; N = 24), or with manual compression with surgical gauze pads (control; N = 23). The proportion of subjects achieving hemostasis at 4 minutes (primary endpoint) as well as at 6 and 10 minutes (secondary endpoints) in the three treatment groups was analyzed using logistic regression analysis, taking into account gender, age, type of intervention, severity of bleeding, systolic blood pressure, diastolic blood pressure, heparin coating of the ePTFE graft, and platelet inhibitors.
RESULTS:
There were substantial differences in the proportion of subjects who achieved hemostasis at the study suture line at 4 minutes from treatment application between FS-120 (62.5%) and control (34.8%) groups (a 79.6% relative improvement). Logistic regression analyses found a statistically significant treatment effect at the 10% level in the odds ratio (OR) of achieving hemostasis at 4 minutes between the FS-120 and control groups (OR = 3.98, p = 0.0991). Furthermore, it has been shown that the perioperative administration of platelet inhibitors significantly influences (OR = 3.89, p = 0.0607) hemostasis rates at the primary endpoint. No statistically significant treatment effects were found for the other factors. Logistic regression analyses performed on the secondary endpoints demonstrated a significant treatment effect of achieving hemostasis at 6 minutes (OR = 9.92, p = 0.0225) and at 10 minutes (OR = 6.70, p = 0.0708) between the FS-120 and control groups. Statistically significant effects in the logistic regression analyses were found at the 10% level in the OR of achieving hemostasis at 6 and 10 minutes, respectively, for the following factors: FS-120 versus control group (OR = 9.92; p = 0.0225 and OR = 6.70; p = 0.0708, respectively), type of intervention (OR = 0.3; p = 0.0775 and OR = 0.25; p = 0.0402, respectively), and heparin coating of the ePTFE prosthesis (OR = 4.83; p = 0.0413 and OR = 3.65; p = 0.0911, respectively). FS was safe and well-tolerated, as indicated by the lack of any related serious adverse events.
CONCLUSION:
The findings from this phase 2 study support the strong safety profile of FS and suggest that it is an efficacious hemostatic agent in ePTFE graft placement surgery, as well as a useful tool in peripheral vascular surgery applications.
18
项与 FS-120 相关的新闻(医药)2024-11-08
摘要:双特异性抗体(bsAbs)能够实现传统基于IgG的抗体无法达到的新型作用机制和/或治疗应用。因此,这些分子在过去十年中引起了极大的兴趣,并且截至2023年底,已有14种bsAbs获得批准:11种用于治疗癌症,3种用于非肿瘤学指征。bsAbs有不同格式,针对不同的目标,并通过不同的分子机制介导抗癌功能。在这里,我们提供了bsAbs在癌症治疗领域最新进展的概述。我们专注于已批准或处于临床开发中的bsAbs,包括bsAb介导的信号通路双重调节剂、肿瘤靶向受体激动剂、bsAb-药物偶联物、双特异性T细胞、自然杀伤细胞和先天免疫细胞的招募者,以及双特异性检查点抑制剂和共刺激因子。最后,我们对处于更早开发阶段的下一代bsAbs进行了展望,包括三特异性抗体、bsAb前药、诱导肿瘤目标降解的bsAbs以及作为细胞因子模拟物的bsAbs。
引言
bsAbs用于双重受体抑制 bsAbs用于配体-受体抑制 bsAbs用于受体激活 bsAbs用于靶向载荷递送 bsAbs用于癌症免疫治疗、 新兴概念 、展望,双特异性抗体通过新生儿Fc受体(FcRn)循环利用。Fc部分的突变可以改变与FcRn的结合,从而改变抗体的半衰期。在不包含Fc部分的bsAbs中,可以通过其他方式实现类似IgG的药代动力学,例如结合到人血清白蛋白(HSA)或其他可以延长半衰期的分子。目前有超过几百种不同类型的bsAb格式,其中多种格式在已批准和处于临床开发中的分子中使用。目前,大多数已批准的bsAbs和处于药物开发高级阶段的分子主要用于癌症免疫治疗。其他针对新型药物递送的实体也在开发中,例如基于bsAb的抗体-药物偶联物(bsADCs)或双重靶向与癌症相关的信号通路(图1)。我们最近在ClinicalTrials.gov、Cortellis和The Antibody Society的数据搜索显示,有超过200种不同的双特异性分子的300多项临床试验正在进行中,其中约75%用于治疗实体瘤,25%用于治疗血液恶性肿瘤(图1)。目前有十种bsAb药物已获批准用于癌症治疗,其中九种在美国和/或欧洲获批准,卡多尼利单抗在中国获批准。在这十种bsAbs中,有九种可以归类为TCEs。卡塔莫单抗是首个获批准的bsAb,于2013年退出市场(表1和图2)。值得注意的是,今天在临床开发中的相当一部分bsAbs已经处于后期阶段(第二阶段和第三阶段)。我们发现,用于治疗实体瘤的bsAbs主要由免疫调节剂主导,包括双重CPIs(约45%)和TCEs(约33%),其次是针对双重通路的bsAbs、ICEs和双重ADCs。相比之下,TCEs是用于治疗血液恶性肿瘤的主要bsAbs类别(约75%),其次是ICEs、双重CPIs和NKCEs(图3)。我们数据集中的bsAbs针对60多个不同的目标,使用超过50种不同的bsAb格式,涉及100多种目标组合。然而,我们承认,该领域的增长速度很快,新的bsAbs,可能具有新的目标和格式,已经进入临床试验,自我们分析以来。尽管如此,本综述旨在提供一份基于MoA的全面概述,介绍作为癌症治疗开发的bsAbs的最新进展,重点关注截至2023年底在同行评审出版物中描述的bsAbs。
双受体抑制的bsAbs
许多参与细胞信号传导的细胞表面蛋白,如RTKs及其相关受体,是抗体基疗法的验证目标。几十年前,对这些蛋白的研究,包括历史上的先行者表皮生长因子受体(EGFR;也称为HER1)、HER2、血管内皮生长因子(VEGF)和针对它们的抗体,为几乎所有后续的抗体基治疗发展奠定了基础。尽管结合一个定义的信号实体的抗体基疗法相当有效,但与疾病相关的表现型通常由多个通路触发。这种冗余允许细胞通过使用其他补偿性信号通路来克服单一目标或通路的药理学生长抑制或诱导细胞毒性。同时调节不同的与疾病相关的信号受体和/或通路的bsAbs可以减少或克服这种限制。Amivantamab(JNJ-61186372)靶向EGFR和肝细胞生长因子受体(MET)。两种受体都会触发非小细胞肺癌(NSCLC)的增殖,因此,阻断两者可以比仅阻断一个通路更有效地抑制NSCLC的生长。Amivantamab已获批准用于治疗携带EGFR外显子20插入突变的NSCLC亚型。
图1 | 用于癌症治疗的双特异性抗体在临床开发中。目前有200多种双特异性抗体(bsAbs)正在进行临床开发,根据癌症类型、临床阶段和作用模式进行分组。正在进行临床开发的bsAbs中有50%处于II期和III期或已经获批。大约四分之三的bsAbs被开发用于治疗实体瘤,实体瘤治疗主要由T细胞招募剂(TCEs;32.9%)和具有检查点抑制和/或免疫调节作用机制(MoAs)的bsAbs(45.1%)所主导。相比之下,血液系统恶性肿瘤的治疗主要由TCEs(75%)和其他MoAs(21.9%)所主导,这些MoAs涉及免疫学活动,如通过检查点抑制和/或免疫调节激活自然杀伤细胞和其他免疫细胞,这归功于高度肿瘤选择性或谱系特异性抗原的可用性。值得注意的是,约有10%用于实体瘤治疗的bsAbs采用双重信号抑制。迄今为止,正在开发的bsAb抗体-药物偶联物(ADCs)用于治疗实体瘤。CPI,检查点抑制剂;ICE,先天细胞招募剂;NKCE,自然杀伤细胞招募剂。
双特异性抗体用于配体-受体抑制
受体激活可以通过干扰受体二聚体化或复合物形成,或通过阻断受体的配体结合位点来抑制。在癌症中,通常来自几个互补或补偿通路的配体和受体有助于肿瘤进展和治疗抗性。bsAbs可以同时阻断两种不同的配体,无论是可溶的还是细胞膜结合的,或者是配体和受体的组合。这种方法不仅用bsAbs来解决,也用双特异性或双位点基于支架的结合剂来解决,这里我们不包括。双重靶向VEGF和血管素2(ANG2)以阻断分别参与血管生成的VEGFR和血管素-1受体(TIE2)的激活,已成为包括微转移的血管生成转换在内的实体瘤中几项临床试验的主题。BI836880是一种三特异性纳米抗体(Nb)融合蛋白,由三个靶向VEGFA、ANG2和HSA的纳米抗体组成,后者用于延长其血清半衰期。这种化合物目前正在对头颈鳞状细胞癌、NSCLC和其他实体瘤患者进行I期研究。值得注意的是,vanucizumab,一种靶向VEGFA和ANG2的bsAb,在与化疗联合使用的临床前模型中显示出抗肿瘤、抗血管生成和抗转移效应,但在与化疗联合使用时,并未在结直肠癌患者中提高无进展生存期,超过VEGF抑制。将VEGF抑制与另一种拮抗活性相结合的概念进一步应用于靶向VEGF和Delta样规范Notch配体4(DLL4)的bsAbs。DLL4是一种细胞表面配体,激活Notch-1受体通路,该通路在肿瘤血管生成中起着核心作用。几种靶向VEGF和DLL4的双特异性抗体已经进入临床试验,包括navicixizumab、dilpacimab和CTX009/ABL001。Navicixizumab是一种四价双特异性抗体,具有四个结合位点,其中两个基于单链可变片段(scFv)融合,它在与紫杉醇联合使用时在铂类耐药卵巢癌患者中展示了有希望的临床活性,并具有可管理的毒性,表明这种方法可能在某些适应症中提供临床益处。相比之下,另一项针对四价双特异性抗体dilpacimab的II期研究,与亚叶酸、氟尿嘧啶和伊立替康(FOLFIRI)联合使用,揭示了安全问题。
表1 | 批准用于癌症治疗的双特异性抗体
ADCC,抗体依赖性细胞毒性;ALL,急性淋巴细胞性白血病;BCMA,B细胞成熟抗原;BiTE,双特异性T细胞招募剂;bsAb,双特异性抗体;DLBCL,弥漫性大B细胞淋巴瘤;EGFR,表皮生长因子受体;EpCAM,上皮细胞粘附分子;GPRC5D,G蛋白偶联受体C类5成员D;MoA,作用机制;NSCLC,非小细胞肺癌;NHL,非霍奇金淋巴瘤;scFv,单链可变片段;TCR,T细胞受体;TDCC,T细胞依赖性细胞毒性。批准区域限于美国、欧洲联盟(EU)、日本和中国;产品也可能在其他国家获得批准。状态截至2023年底。
靶向VEGF和PDL1或PD1的双特异性抗体
基于VEGF抗体和免疫检查点抑制剂(CPI)联合治疗的积极结果,上述概念进一步适应于设计靶向VEGF和肿瘤细胞上的PDL1或T细胞上的PD1的双特异性抗体,从而将抗血管生成与免疫肿瘤学方法相结合。使用这种方法最先进的分子是ivonescimab(AK112),它针对PD1和VEGF。目前,ivonescimab的上市申请正在中国接受监管审查。其他双特异性抗体靶向PDL1和VEGF,包括PM8002,目前正在进行II/III期研究(NCT05756972),针对NSCLC患者。
受体激活的双特异性抗体
许多抗肿瘤反应是通过激活细胞表面受体介导的,包括免疫反应或通过诱导凋亡的细胞死亡。癌症治疗的一种方法是通过将受体激活配体(如生长因子、细胞因子和(共)免疫刺激配体)融合到抗体或抗体片段上,实现受体激活配体的靶向递送,以诱导局部或组织特异性的激动活性,从而引发细胞反应。越来越多的这些抗体-配体融合蛋白正在进入临床试验。受体激活也可以通过激动性抗体来实现。肿瘤坏死因子(TNF)超家族的成员,包括死亡配体(如TNF配体超家族成员10(TNFSF10);也称为TRAIL)及其各自的死亡受体(如TRAIL受体1和2;也称为DR4和DR5),或具有免疫细胞共刺激活性的配体(如TNFSF9;也称为4-1BBL)及其受体(如TNFRSF9;也称为4-1BB或CD137)在癌症治疗中引起了特别关注。然而,单克隆抗体在临床试验中取得了相当令人失望的结果。原因是许多TNFRSFs需要超过两个受体的交联以激活,这只能通过Fc-FcγR介导的抗体在细胞表面的超聚集来实现,因此依赖于TME中表达足够数量FcγR的先天免疫细胞。作为替代方案,针对目标抗原和TNFRSF成员的双特异性抗体已被证明可以作为强大且肿瘤选择性的激动分子,模仿表面展示配体的活性。这尤其适用于DR4和DR5,DR5需要多个受体的聚集才能激活。值得注意的是,针对DR5和表面抗原的双特异性抗体,如成纤维细胞激活蛋白-α(FAPα;也称为脯氨酸内肽酶FAP)、钙粘蛋白17(CDH17)或叶酸受体-α(FRα),不仅有效地诱导受体激活,还避免了通过诱饵受体的隔离50。RG7386(RO6874813),一种针对癌症相关成纤维细胞上的FAPα和DR5的四价双特异性抗体,在体外和体内在表达FAPα的基质的小鼠中触发了强效且选择性的肿瘤细胞杀伤,并已进入临床测试,但由于战略投资组合优先级而随后中止。此外,BI905711,一种针对DR5和CDH17的四价双特异性IgG-scFv融合蛋白,目前正在进行I期临床研究,显示出在CDH17阳性目标细胞上的效力比单克隆抗体提高了1000倍以上,转化为在结直肠癌模型中的强效且选择性的抗肿瘤活性。相同的格式用于针对DR5和FOLR1的双特异性抗体,FOLR1是一种富集于卵巢癌的受体,已被证明介导顺式(在同一细胞上)和反式(在两个不同细胞上)的细胞毒性,其中FOLR1作为有效DR5激活的聚集点。从概念上讲,这种MoA也可以转移到依赖于受体聚集的TNFRSF家族的共刺激成员,包括4-1BB、OX40和CD40(见图3),使用针对肿瘤相关抗原(TAAs)的双特异性抗体,但也针对其他目标,如PDL1,从而将共刺激与检查点抑制相结合(见下文)。
用于靶向载荷递送的双特异性抗体
存在两种概念上不同的方法,用于使用双特异性抗体进行有效载荷(如细胞毒素或放射性)的靶向递送。第一种方法,预靶向治疗,使用双特异性抗体的一个结合特异性来靶向肿瘤细胞,另一个结合特异性随后捕获肿瘤上的载荷。这类双特异性抗体结合到肿瘤上的癌症靶标,如癌胚抗原(CEACAM5)或HER2,然后捕获由双特异性抗体的第二个结合特异性识别的放射性标记载荷/复合物。
图2 | 已批准用于癌症治疗的双特异性抗体概览。a, 双特异性T细胞招募剂(TCEs)。b, 其他双特异性抗体(bsAbs)(非T细胞招募剂(非TCEs))。11种已批准的bsAbs中有6种具有IgG样结构,由2条重链(恒定区域以深灰色显示,Vh结构域以深蓝色或深红色显示)和2条轻链(恒定结构域以浅灰色显示,Vl结构域以浅蓝色或浅红色显示)组成。它们大多数具有1+1的化学计量比 —— 每个抗原一个结合位点 —— 还有一个TCE通过将一个额外的Fab片段融合到一条重链上,利用2+1的化学计量比。其他的bsAbs要么是不含Fc的融合蛋白,由两个单链可变片段(scFv)片段组成(blinatumomab),要么是将scFv片段与T细胞受体(TCR)片段融合,或者是具有2+2化学计量比的IgG-scFv融合蛋白。除了由小鼠和大鼠杂交瘤细胞技术生产的catumaxomab外,所有其他的bsAbs都是通过重组技术生产的。对于IgG样异二聚体分子,通过在CH3域使用突变来强制异二聚体化 —— 如旋钮-入洞技术 —— 或控制的Fab臂交换(cFAE),解决了两种不同重链的正确组装问题,cFAE还允许从两种不同的单特异性IgG组装IgG样分子。cFAE还解决了轻链问题,即轻链和重链的配对。或者,如CrossMab方法所示,对Fab臂进行进一步的修改,以强制正确的轻链和重链配对。值得注意的是,所有重组IgG样bsAbs都包含一个具有沉默或减少效应功能的Fc区域,这是通过在铰链/CH2域引入突变来避免或减少Fcγ受体和补体结合来实现的。BCMA,B细胞成熟抗原;EGFR,表皮生长因子受体;EpCAM,上皮细胞粘附分子;GPRC5D,G蛋白偶联受体C类5成员D。
最近,被称为SADA的双特异性抗体利用改良的p53四聚体化域来延长GD2×DOTA在肿瘤中的滞留时间。GD2×DOTA是一种双特异性抗体,能够识别在癌症中高表达的二唾液酸神经节苷脂GD2,以及放射性载荷177Lu-DOTA,在肿瘤微环境中组装并滞留在那里,但没有四聚体化,它会迅速从周围清除,因为它缺乏半衰期延长。到目前为止,很少有临床试验中的双特异性抗体使用这种MoA,可能是由于与预靶向放射性相关的复杂物流限制了其普遍适用性。
图3 | 目前正在临床试验中的双特异性抗体的作用机制。a, 通过受体阻断两种不同的信号受体(以不同颜色表示)来抑制信号传导。b, 通过抑制可溶性配体(蓝色)和受体来抑制信号。c, 通过双重阻断两种不同的配体来抑制信号。d, 通过双特异性抗体(bsAb)药物偶联物(偶联物以浅蓝色表示)进行药物传递。e, 针对性阻断“别吃我信号”(CD47–SIRPα相互作用),导致巨噬细胞的吞噬作用。f, 结合检查点抑制,阻断“别吃我信号”。g, 通过T细胞受体(TCR)上的CD3或自然杀伤细胞上的CD16(FcγRIIIa)激活效应细胞。h, 肿瘤细胞结合介导的免疫细胞(共)刺激。i, PDL1结合介导的免疫细胞(共)刺激。j, 双重免疫细胞共刺激。k, 肿瘤靶向PDL1途径抑制。l, 肿瘤靶向PD1途径抑制。m, 检查点结合介导的免疫细胞(共)刺激。n, 双重检查点抑制。o, 通过配体阻断实现双重检查点和可溶性转化生长因子-β(TGFβ)信号的抑制。展示了用于实体瘤和血液系统恶性肿瘤的目标分子和肿瘤相关抗原(TAAs)的例子。注意:bsAbs可以同时发挥多种作用机制(MoAs)。Ang2,血管生成素2;APC,抗原呈递细胞;BCMA,B细胞成熟抗原;CDH17,钙粘蛋白17;DLL4,典型Notch配体4;EGFR,表皮生长因子受体;EpCAM,上皮细胞粘附分子;FRα,叶酸受体α;GPRC5D,G蛋白偶联受体C类5成员D;HLA,人类白细胞抗原;ICOS,诱导性T细胞共刺激因子;LAG3,淋巴细胞相关基因3;TIGIT,具有免疫球蛋白和ITIM结构域的T细胞免疫受体;VEGF,血管内皮生长因子。
双特异性抗体药物偶联物
第二种方法通过同时靶向肿瘤细胞表面的两个表位或两个目标,实现了通过双特异性抗体药物偶联物(bsADCs)传递细胞毒素载荷的特异性靶向。处于临床开发中的bsADCs的例子包括zanidatamab zovodotin(ZW49),这是一种双特异性HER2结合抗体zanidatamab与auristatin衍生的细胞毒素载荷偶联,双特异性MET×MET bsADC REGN5093或izalontaxab brengitecan(BL-B01D1),一种EGFR×HER3 bsAb与一种新型TOPO-I抑制剂偶联(NCT05194982)(表2)。
双特异性抗体用于癌症免疫治疗
大多数用于癌症免疫治疗的双特异性抗体通过T细胞驱动的自然或内源性免疫发挥作用,例如通过增强现有的抗肿瘤反应和/或克服检查点抑制,或通过提供合成免疫,例如通过bsAb驱动的免疫细胞的参与、激活和招募(图3)。在这一部分中,我们提供了包括CPIs、效应细胞招募剂(包括TCEs和ICEs)和共刺激双特异性抗体在内的最突出的MoAs的概述。
双重CPIs
许多干扰免疫检查点(如CTLA4或PD1/PDL1)的单特异性抗体已获批准用于癌症免疫治疗,包括ipilimumab、tremelimumab、nivolumab、pembrolizumab、atezolizumab、avelumab、durvalumab或cemiplimab。将免疫检查点抑制抗体治疗扩展到包括双特异性抗体可能会减少不良副作用并提高观察到的单特异性抗体治疗的疗效。第一个方面,检查点抑制的安全性,包括预防自身免疫相关事件和/或不希望的免疫细胞激活。为了实现这一目标,正在开发针对检查点抑制功能和TAAs(如RTKs)的双特异性抗体,目的是将其活动更优先地集中在肿瘤上,正在开发中。第二个方面,检查点免疫治疗的疗效,通过双特异性抗体同时靶向两种不同的检查点蛋白来提高疗效并降低抗性的可能性,或提供互补的免疫刺激信号。值得注意的是,这些双特异性抗体的共同设计原则是提高对表达两种检查点蛋白的T细胞的选择性,如CTLA4/PD1或PD1/淋巴细胞相关基因3(LAG3),这些蛋白可能更具肿瘤反应性,目标是提供比单独检查点阻断更优越的治疗指数。
表2 | 晚期临床开发中选择的双特异性抗体概览
BiTE,双特异性T细胞招募剂;BCMA,B细胞成熟抗原;bsAb,双特异性抗体;BTC,胆管癌;cL,普通轻链;DART,双亲和重定向;DLL4,类似Delta的典型Notch配体4;EGFR,表皮生长因子受体;EpCAM,上皮细胞粘附分子;Fchet,异二聚体化Fc;LAG3,淋巴细胞相关基因3;Nb,纳米抗体;NHL,非霍奇金淋巴瘤;NSCLC,非小细胞肺癌;PDC,胰腺导管腺癌;scFv,单链可变片段;TIGIT,具有免疫球蛋白和ITIM结构域的T细胞免疫受体;TGFβ,转化生长因子β;VEGF,血管内皮生长因子。a晚期包括关键性II期、II/III期和III期临床研究。
例如,通过降低自身免疫不良事件的发生率 —— 而不是与联合检查点阻断相比。探索肿瘤靶向检查点抑制的工作包括开发双特异性抗体,这些抗体靶向肿瘤细胞表面的HER家族RTKs,并结合PD1/PDL1信号通路的阻断作为第二功能,从而将PDL1结合剂定向到肿瘤细胞。这些分子的特定肿瘤靶向导致了对表达EGFR的肿瘤细胞更具特异性和增强的活性。类似地,一种特别结合HER2和PDL1的双特异性抗体被证明可以在HER2表达的肿瘤细胞中特异性阻断PDL1活性,从而比单独使用每个实体或在不作为双特异性抗体结合时联合应用产生更大的治疗效果。
另一种双特异性抗体介导的靶向免疫治疗方法包括将PDL1阻断与识别黑色素瘤上的软骨素硫酸蛋白聚糖4(CSPG4)的结合物相结合。特定的肿瘤靶向增强了抗肿瘤T细胞的特异性、激活状态和疗效。概念上相关的方法包括将PDL1结合物与黑色素细胞刺激激素化学偶联。通过这种方式,PDL1抑制活性被定向到黑色素瘤细胞上的黑色素皮质素-1受体。同时靶向两个检查点蛋白而不额外包括常见的肿瘤细胞表面靶标的双特异性抗体的例子包括同时结合肿瘤细胞上的PD1和PDL1的双特异性抗体。Wan等人分析了这种双特异性抗体在高级别浆液性卵巢癌类器官与免疫细胞共培养中引发的联合活性。与单特异性结合物相比,双特异性抗体介导了优越的疗效,并在T细胞和自然杀伤细胞中诱导了表型变化,包括激活状态和细胞毒性的改变。双特异性抗体LY3434172也采用了这种方法。通过完全抑制PD1/PDL1途径,LY3434172显示出比每个亲本抗体或两者组合更大的抗肿瘤活性,再次证明以双特异性抗体形式的结合很重要,并且可以增加疗效。超越PD1/PDL1方法的界限,包括CTLA4在内的其他免疫受体的双特异性抗体正在开发或已获批准。同时靶向PD1和CTLA4是双特异性抗体cadonilimab的作用机制。Cadonilimab由于四价性,介导了对高密度PD1和CTLA4的增加亲和力驱动的目标结合,这与Fc突变以废除FcγR结合相结合,可能是其有利的治疗指数的基础。值得注意的是,cadonilimab还在PD1+和CTLA4+ T细胞之间介导了跨结合。在晚期实体瘤患者的I/Ib期研究中,cadonilimab显示出抗肿瘤活性和有利的安全性概况,免疫相关不良事件的发生率低。Cadonilimab已在中国获批准用于治疗在铂类化疗后或化疗期间进展的复发或转移性宫颈癌。其他在高级临床试验中结合相同特异性的双特异性抗体是MGD019和MEDI5752。MGD019结合了PD1和CTLA4结合物,在进行中的临床研究中观察到可接受的安全性和组合阻断以及在多种实体瘤中的客观反应。MEDI5752目前正在进行临床评估,它结合了PD1和CTLA4,并显示了PD1介导的靶向,因为它优先饱和了PD1+ T细胞上的CTLA4,并引起了PD1的快速内化和降解。与cadonilimab相比,MGD019和MEDI5752似乎对双阳性T细胞显示出更强的亲和力驱动的选择性增益。双重失活也在探索中,通过结合PD1/PDL1阻断与LAG3或TIM3抑制。例子是IBI323和FS118,它们都结合了PDL1和LAG3,并在临床前模型中显示出增强的双重功效。LY3415244结合了PDL1和TIM3的阻断,作为一种不同的免疫调节剂,但由于在I期研究中观察到的免疫原性,该分子的开发被终止。最近,I期剂量递增和扩展数据的临床试验显示,PD1×LAG3双特异性抗体tebotelimab在实体瘤或血液系统恶性肿瘤患者中作为单药治疗以及与HER2抗体margetuximab联合治疗时显示出有希望的活性。双配体抑制是另一种基于双特异性抗体的检查点抑制方法。PDL1和转化生长因子-β(TGFβ)是具有互补且非冗余免疫抑制活性的受体结合配体。TGFβ不仅具有免疫抑制作用,还可以进一步诱导促血管生成因子的上调和癌症相关成纤维细胞的激活。目前正在开发几种靶向PDL1和TGFβ的双特异性抗体,如类似双特异性抗体融合蛋白的bintrafusp alfa(M7824)。在这种情况下,PDL1的结合是通过一个“标准”的抗体结合模块实现的,而TGFβ则被人类TGFβ受体II的细胞外域捕获。Bintrafusp alfa在临床前研究中显示了激活先天和适应性免疫系统,从而比单独使用抗PDL1抗体或TGFβ陷阱模块更好地抑制肿瘤生长和转移,目前正在进行临床试验。Retlirafusp alfa(SHR-1701),另一种以类似方式靶向PDL1和TGFβ的双功能融合分子,正在对宫颈癌和胃癌或胃食管结合部癌症患者进行III期研究(表2)。YM101是一种TGFβ×PDL1双特异性抗体,目前处于临床前开发阶段。YM101的一个替代品,Y101D,正在对晚期实体瘤患者进行评估(NCT05028556)。所有同时对抗抑制性TGFβ和PD1/PDL1途径的方法在体内模型中显示出比单独使用各自结合物更高的抗肿瘤活性,但迄今为止尚未在临床上证明概念。针对性的TGFβ信号阻断也已经在临床前研究中通过阻断CD4+ T细胞中的TGFβ信号的双特异性抗体实现。为此,将非免疫抑制性的CD4靶向抗体ibalizumab与TGFβ陷阱以类似于上述的双特异性抗体方式结合。这导致在辅助T细胞中针对性阻断TGFβ信号,可以释放抗肿瘤反应。通过双特异性抗体招募磷酸酶抑制PD1是一种最近报道的新型MoA88。这是通过一个单域(Vhh)融合到一个scFv实现的,将PD1连接到细胞表面磷酸酶CD45,这反过来触发细胞内去磷酸化。这种方法与单独使用PD1抗体介导的配体阻断相比,增强了检查点阻断的抑制。按照同一原则,双特异性抗体可以将细胞表面磷酸酶CD45与抑制性自然杀伤细胞表面受体NKG2A或Ly49连接,以进行后续去磷酸化。这样的双特异性抗体可以阻断并同时去磷酸化它们的目标,可能比相应的单特异性抗体及其抑制信号的组合更有效的拮抗剂,以增强自然杀伤细胞和T细胞的抗肿瘤活性。使用双特异性抗体对CD73的不同表位进行双位点靶向是另一种双特异性抗体相关方法,以抵消免疫抑制活性或增强针对肿瘤的免疫能力。CD73产生免疫抑制性腺苷,其通过内化的双特异性抗体介导的抑制和耗尽比单一位点CD73抗体更有效。
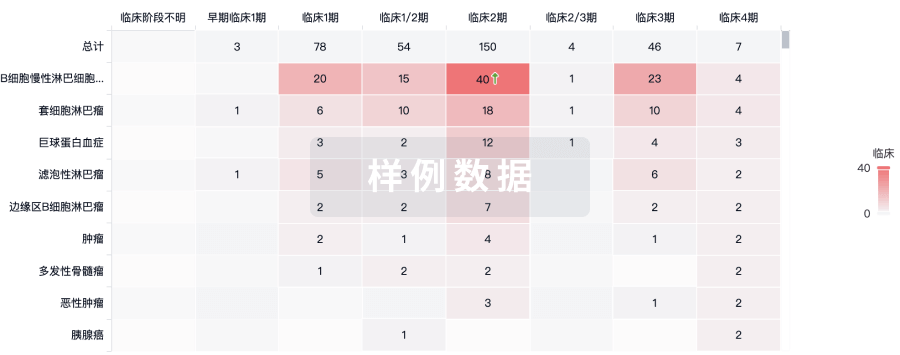
效应细胞招募剂 T细胞招募剂
在过去二十年中,专门结合肿瘤表面抗原和TCR的CD3ε链的T细胞招募剂(TCEs)在这一类双特异性抗体中占据主导地位,描述了数百种TCEs,并且有100多种进入临床开发。事实上,第一个获准上市的双特异性抗体是鼠/大鼠嵌合的上皮细胞粘附分子(EpCAM)×CD3ε双特异性抗体catumaxomab,它在2009年被欧洲联盟(EU)批准用于恶性卵巢腹水的腹腔内治疗,但后来因商业原因退出市场。目前正在中国再次进行临床试验,用于腹腔内给药。系统应用的catumaxomab显示出严重的输注反应和高免疫原性发生率,可能由于其鼠/大鼠嵌合的恒定区域和保留的FcγR结合,导致在没有抗原结合的情况下非特异性FcγR和TCR激活。随后,下一代TCEs被设计为缺乏Fc部分,如基于串联scFv的CD19×CD3ε双特异性T细胞招募剂(BiTE)blinatumomab,它在2014年首次被批准用于治疗B细胞前体急性淋巴细胞性白血病(B-ALL)。然而,由于缺乏通过FcRn的循环,这种疗法需要持续输注,FcRn通过从分拣内体循环到细胞表面,从内溶酶体降解中挽救IgG。基于blinatumomab的成功,针对血液和实体瘤的各种目标的BiTEs被开发出来,但最终没有进入晚期临床试验,由于BiTEs和相关短半衰期的药代动力学特性不佳。人们尝试通过纳入FcγR结合惰性Fc结构域(沉默Fc)或HSA结合部分来实现bsAbs的IgG样半衰期,目前大多数处于开发中的TCEs是基于IgG和/或具有IgG样药代动力学的。值得注意的是,大多数TCEs使用单个单价结合位点用于CD3作为T细胞上的触发分子,以避免在没有同时目标结合的情况下TCR交联引起的系统性T细胞激活。然后它们使用一个(1+1)或两个(2+1)肿瘤目标的结合位点,因为双价结合可以在肿瘤选择性和效力方面提供优势。CD20×CD3ε双特异性抗体mosunetuzumab106和B细胞成熟抗原(BCMA)×CD3ε双特异性抗体teclistamab是第一批异二聚体1+1 IgG基TCEs,分别在2022年被批准用于治疗复发/难治性滤泡性非霍奇金淋巴瘤(NHL)或多发性骨髓瘤。在2023年,异二聚体2+1 CD20-TCE glofitamab104,108和1+1 CD20-TCE epcoritamab109被批准用于治疗复发/难治性弥漫大B细胞淋巴瘤(DLBCL),以及1+1 G蛋白偶联受体C类5成员D(GPRC5D)-TCE talquetamab110和BCMA-TCE elranatamab111用于复发/难治性多发性骨髓瘤(表1)。CD20-TCE odronextamab112和BCMA-TCE linvoseltamab的上市申请正在等待监管决定。鉴于它们在复发/难治性B细胞和浆细胞恶性肿瘤患者中显示出的有希望的临床疗效和完全缓解率 —— 包括在CAR-T细胞治疗后复发的患者中的活性 —— 以及它们作为现成疗法的简单可用性以及皮下给药的可能性,可以预期TCEs将成为CAR-T细胞疗法的主要替代品,特别是随着它们开始被开发用于更早期的治疗线并且可以让患者轻松获得。免疫动员单克隆T细胞受体针对癌症(ImmTACs)是结合了工程化TCR以识别人类白细胞抗原(HLA)呈递的肽抗原与抗CD3 scFv的TCEs,实现对细胞内TAAs的靶向。值得注意的是,短暂存在的ImmTAC tebentafusp,它包含一个针对由HLA-A*02:01呈递的黑色素细胞谱系特异性抗原糖蛋白(gp100)表位的可溶性TCR融合到CD3靶向scFv,已在2022年被批准用于治疗葡萄膜黑色素瘤,为TCEs在实体瘤中的细胞内靶标空间开辟了新的领域。值得注意的是,tebentafusp介导了总体生存益处,尽管它只诱导了少数临床反应,因此直接杀死肿瘤细胞可能不是其唯一的MoA。与此同时,各种基于重组TCR或使用类似TCR的抗体(TCR模拟物)的TCEs已进入临床开发,包括针对WT1和突变新抗原如KRAS122或p53的TCEs。重要的是,高通量动力学筛选和通用TCR类似库可以促进高度选择性的TCR和TCR模拟物的开发,用于TCEs。有趣的是,使用共价KRASG12C抑制剂sotorasib,可以产生一种类似TCR的TCE,可以特异性识别HLA呈递的sotorasib-肽共轭物,并随后诱导KRASG12C突变细胞的T细胞杀伤。细胞因子释放综合征的发生,主要是由于靶向T细胞激活,一直是TCEs临床开发的一个主要挑战。尽管在许多情况下,这可以通过使用类固醇预处理和逐步剂量增加来管理,但最近的努力已经研究了使用具有降低CD3ε亲和力的CD3ε抗体,目标是将T细胞杀伤与细胞因子分泌解耦。与CAR-T细胞一样,由于TCEs的杀伤效力非常高,因此需要严格肿瘤特异性和/或谱系特异性表达目标抗原,以避免靶向非肿瘤毒性。对于血液癌症中的B细胞和浆细胞抗原,如CD19、CD20、CD79b、BCMA140141和FcRH5,通常认为它们只存在于B细胞和浆细胞恶性肿瘤以及非必需的B细胞和浆细胞谱系中。然而,即使对于CD19等抗原,其在正常组织中的表达可能并非绝对不存在,有报道称CD19在围绕内皮细胞的壁细胞/血管周细胞上表达,这些细胞对血脑屏障完整性至关重要,作为一种靶向非肿瘤机制与神经毒性有关。相比之下,在急性髓系白血病中,典型的抗原如CD33或CD123也存在于髓系造血谱系上,使得它们的临床开发更具挑战性。类似地,许多主要的(上皮)实体瘤抗原如EGFR、HER2、EpCAM、肿瘤相关钙信号转导蛋白2(也称为细胞表面糖蛋白Trop-2)、MUC1、CEACAM5和glypican 3也可以在(必需的)正常组织中找到。因此,由于更免疫抑制性的肿瘤微环境,TCEs(和CAR-T细胞)在实体瘤的开发在过去几年中进展较少。重要的是,必须认识到对于TCEs,与ADCs150相比,由于更高的效力,对肿瘤选择性的要求更严格,固体瘤ADC靶标如HER2和TROP-2可能无法用传统的TCEs靶向。与此同时,与TCEs相比,ADCs可能由于在肿瘤微环境中释放有毒载荷而受益于更强的旁观者杀伤效应,对抗原阴性肿瘤细胞进行杀伤。因此,很少有肿瘤选择性抗原似乎是TCEs的可行靶标,包括新抗原如p95-HER2和EGFRvIII,或者MUC16、claudin 18.2、DLL3和STEAP1等靶标。对于DLL3靶向的TCE tarlatamab,目前正在美国食品药品监督管理局(FDA)的优先审查中,已在小细胞肺癌中报告了有希望的I期临床数据,总反应率达到23%。随后的II期研究证实了活动性,持久的客观反应和有希望的生存结果,使用每2周10毫克剂量治疗的患者。基于这些数据,已启动了一项随机关键研究,比较tarlatamab与标准护理(NCT05740566)。同样,xaluritamig,一种2+1 STEAP1 TCE,具有亲和力驱动的活性,能够选择性地针对高表达STEAP1的肿瘤细胞与正常细胞相比,已在转移性去势抵抗性前列腺癌患者的I期剂量递增研究中展示了有希望的临床活性。综上所述,这些概念验证数据表明,TCEs仅限于血液癌症活跃的共同假设,特别是B细胞恶性肿瘤,并不适用,并且TCEs也有可能治疗某些实体瘤,只要能够管理靶向非肿瘤活性。正在使用多种方法来克服实体瘤选择性挑战。例如,在双特异性抗体中使用具有降低亲和力的肿瘤抗原结合物(2+1格式)可以实现亲和力介导的选择性增益(也称为亲和力调节),目标是利用肿瘤和正常组织之间的表达差异,如CEACAM5、HER2和FOLR1,以提高肿瘤选择性。或者,双重靶向和亲和力介导的选择性增益应用于三特异性TCEs,这些TCEs选择性地杀死共同表达这些靶标的肿瘤细胞,但不会影响只表达这些靶标中一个的正常细胞。此外,针对两种不同的肿瘤抗原如CD19和CD22的三特异性TCEs可以防止通过抗原丢失的免疫逃逸。尽管大多数传统的TCEs可以招募常规T细胞和非传统先天样γδ T细胞(表达TCRγ/δ而非TCRα/β的T细胞),但一类特定的γδ TCEs已被设计为通过TCRγδ特别招募γδ T细胞,目标是通过只针对可以在患者中进一步扩展的T细胞亚群来提高安全性和有效性。在临床前研究中,γδ TCEs作为单一药物显示出强大的抗肿瘤活性。或者,为了此目的,制造了针对肿瘤的双特异性异二聚体BTN2A1和BTN3A1抗体融合蛋白。由于γδ T细胞生物学在小鼠模型中没有完全反映,这种方法的最终概念验证将不得不依赖于正在进行的临床试验的临床数据,如针对PSMA的γδ TCE LAVA-1207(NCT05369000)。而不是针对CD3ε或TCRα/β的双特异性抗体,肽-MHC复合物可以被应用来特别招募特定pMHC复合物的T细胞,如由于自然发生和普遍的巨细胞病毒感染而存在的巨细胞病毒衍生肽。在另一种方法中,病毒表位可以被传递到肿瘤细胞中,以便加载相应的MHC分子,并招募病毒特异性T细胞攻击这些细胞。还描述了用于更有效介导双特异性抗体介导的聚集和补体依赖性细胞毒性的双特异性抗体。有趣的是,通过应用两对独立的抗体,可以建立一种逻辑门,通过补体依赖性细胞毒性选择性地消除共表达两种抗原的细胞。例如,使用这种方法,可以消除共表达CD20和CD52的B细胞,而单独表达这些抗原的细胞则不会被杀死。随着对采用CAR-T细胞疗法的极大兴趣,一类特定的TCEs,作为CAR-T细胞和肿瘤细胞之间的双特异性适配器,已被设计为特别招募采用转移的T细胞用于治疗各种癌症,同时不涉及自然T细胞。其中一个例子是合成激动性受体(SAR)-T细胞系统,其中一种双特异性抗体识别肿瘤抗原和一个引入到采用转移的T细胞中的合成抗原受体。这种在合成生物学背景下的方法提供了多种方式。
进一步工程化和控制采用T细胞疗法方法,超出了传统抗体疗法或经典CAR-T细胞疗法所能提供的范围。另一种结合细胞疗法和双特异性抗体的方法是体外武装T细胞与多种TCEs,目标是克服肿瘤异质性。为此,T细胞在体外与针对肿瘤抗原如GD2、HER2、PSMA和STEAP1的TCEs孵育,并给药于肿瘤携带动物,在这些动物中,由于抗原丢失,它们阻止了肿瘤进展。
固有细胞招募剂
尽管TCEs在效应细胞招募剂领域占据主导地位,但正在大力开发下一代ICEs,包括NKCEs和双特异性抗体,这些抗体招募髓系衍生细胞(MDCs)进行吞噬作用,包括中性粒细胞和巨噬细胞/单核细胞。介导ADCC的单克隆抗体,如利妥昔单抗、西妥昔单抗或曲妥珠单抗,因为ADCC/抗体依赖性细胞吞噬作用对其MoA至关重要,除了其他作用如信号抑制外,可以被视为第一代ICEs。基于这种经验,已经批准了几种与常规单克隆抗体相比具有增强ADCC功能的Fc工程化IgG1抗体,包括obinutuzumab、mogamulizumab、tafasitamab、margetuximab和amivantamab。基于这种经验和目标,进一步增强ADCC功能,超越Fc工程化IgG1抗体,已经开发了各种双特异性NKCEs,它们针对自然杀伤细胞上的不同表面分子,如CD16、NKG2D、NKp46或NKp30,作为免疫疗法。这些NKCEs中最先进的是一种短半衰期的CD30×CD16双特异性抗体,用于治疗霍奇金淋巴瘤,可以作为单一疗法、与检查点抑制联合或与自然杀伤细胞输注联合使用。最近,开发了针对抗原如EGFR或BCMA的半衰期延长的四价IgG基双特异性抗体,以及利用双重靶向实现肿瘤选择性的三特异性抗体。对称的三特异性NKCEs通过ADCC特别针对通过其CD16结合区域共表达EGFR和PDL1的细胞,使用两种合一抗体技术。另一种激活自然杀伤细胞的方法依赖于双特异性融合蛋白,该蛋白由NKG2D配体(例如UL-16结合蛋白2(ULBP2))与针对HER2的scFv融合,以实现有效的ADCC介导的肿瘤细胞杀伤。或者,保留FcγRIII结合的双特异性抗体,针对NKp46或NKp30和各种肿瘤抗原,可以提供强大的抗肿瘤效果。与TCEs不同,其中FcγR结合是不需要的,这些双特异性抗体依赖于保留或增强的FcγRIII结合,以实现有效的自然杀伤细胞参与。值得注意的是,当IL-2变体被融合到NKp46双特异性抗体上,产生四功能分子时,由于同时诱导自然杀伤细胞扩增,效果大大增强。另一个积极研究的领域是双特异性抗体,这些抗体通过结合,例如,巨噬细胞和中性粒细胞上的FcαRI受体(CD89)或通过双特异性IgE抗体的IgE受体,参与吞噬作用或MDCs以及中性粒细胞的杀伤。或者,肿瘤靶向双特异性抗体可以阻断肿瘤细胞上基于'不要吃我信号'的CD47–SIRP1α相互作用,以便这些细胞被MDCs攻击和吞噬。双特异性CD19 x CD47或间皮素x CD47抗体结合了肿瘤靶向和CD47抑制以及通过效应功能完整的Fc部分招募效应细胞。在这种情况下,对CD47具有低亲和力的双特异性抗体有利于克服不必要的结合到红细胞上的CD47。
各种团队应用这一概念进行PDL1×CD47共靶向。或者,SIRPα融合蛋白可以用来阻断CD47–SIRPα“不要吃我”信号。
共刺激双特异性抗体
有效、持久且局部限制的抗肿瘤免疫反应需要共刺激和共抑制信号来紧密调节细胞毒性T细胞、自然杀伤细胞和巨噬细胞的激活、分化和维持。TNFRSF家族成员(如4-1BB、CD40、OX40、TNFRSF18(也称为糖皮质激素诱导的TNFR相关蛋白(GITR))、CD27或CD30)以及CD28免疫球蛋白超家族(如CD28、CTLA4、PD1、诱导性T细胞共刺激因子(ICOS)和B淋巴细胞和T淋巴细胞衰减因子(BTLA))及其相应的配体,在通过细胞-细胞接触(如抗原呈递细胞(APCs)和T细胞之间)提供的局部免疫调节信号中发挥着显著作用。这些受体为T细胞提供了所谓的信号2,这对于维持TCR通过肽-MHC-TCR相互作用或通过TCE交联TCR所提供的信号1是必需的。针对这些免疫调节途径的靶向可能增强免疫疗法。研究表明,针对共刺激受体的激动性单克隆抗体通常只会导致微弱的激活,但这种激活可以通过FcγR介导的受体超聚集显著增加。此外,抗体与受体之间的化学计量比、结合亲和力和表位特异性等因素可以影响共刺激抗体的活性。因此,降低免疫调节抗体的亲和力可以作为一种策略,通过增加受体聚集来增强激动性活性,这一原则经常应用于双特异性抗体激动剂(见上文)。然而,由于增加的趋化因子和细胞因子产生导致的免疫相关系统性不良事件是共刺激抗体药物开发的限制因素。抗体-细胞因子融合蛋白和双特异性抗体能够以目标依赖的方式提供共刺激信号,通过双重靶向两种不同的共刺激受体或通过靶向共刺激受体和CPI来规避这一限制。
肿瘤靶向共刺激双特异性抗体
用一个臂结合到TAA上,另一个臂结合到免疫细胞上的共刺激受体上的双特异性抗体,可以通过在癌细胞和免疫细胞之间跨作用来局部介导受体聚集,从而提供信号2。目前正在临床试验中的共刺激双特异性抗体包括针对4-1BB、CD40和CD28的分子。T细胞激活后诱导表达的4-1BB使其成为增强CD8 T细胞反应的T细胞共刺激的有吸引力的靶标。使用针对4-1BB的激动性抗体(如urelumab和utomilumab)作为单一疗法在临床试验中的安全性问题和较差的疗效,使人们重新将努力集中在可以克服这些毒性的双特异性抗体上,通过引入肿瘤特异性共刺激。大约一半的癌症靶向共刺激双特异性抗体在临床试验中通过4-1BB发挥作用。先进的双特异性抗体包括PRS-343(cinrebafusp),一种针对HER2和4-1BB的四价双特异性抗体-抗钙蛋白融合蛋白,在IND使能研究中被发现耐受性良好,没有明显和相关药物相关毒性;FAP-4-1BBL(RG7872),作为单一疗法和与PDL1抑制联合使用时显示出药理活性;或englumafusp alfa,正在研究中作为与glofitamab联合用于DLBCL的信号2提供者。其他在临床试验中通过4-1BB进行肿瘤选择性共刺激的双特异性抗体目标包括EGFR、PSMA、CLDN18.2、B7H4、CEACAM5、HER2、PDL1(见下文)和FAP48。此外,使用CD28作为共刺激受体的双特异性抗体,目前在临床试验中。通过与APC上的CD80(也称为B7.1)或CD86(也称为B7.2)的结合,CD28为幼稚T细胞提供了必要的二次信号,以实现完全的T细胞激活和存活。这种信号也可以通过激动性CD28抗体提供,即使在没有初级TCR参与的情况下,如超激动剂TGN1412所示,它在I期研究中因大量细胞因子释放综合征而显著失败。后来发现,TGN1412特别在低剂量下作用于调节性T细胞(Treg细胞),而在高剂量下激活传统T细胞和Treg细胞,为选择性靶向T细胞亚群提供了窗口,但也突出了T细胞共刺激与超激活之间的微妙平衡。一些双特异性抗体可以以目标依赖的方式提供这种二次共刺激信号,以增强肿瘤限制性的抗肿瘤T细胞反应。值得注意的是,双特异性抗体可以被设计为单独使用时活性有限且无毒性,但可以增强T细胞激活和TCEs的抗肿瘤活性。REGN5837是一种针对CD22和CD28的双特异性抗体,已进入与针对CD20的TCE odronextamab联合用于NHL治疗的I期试验。肿瘤靶向CD28双特异性抗体也可以与PD1协同作用,提供长期抗肿瘤免疫反应,目前,多个针对TAAs如EGFR、MUC16、PSMA、B7-H3、CD19、CD22或PDL1的双特异性抗体正在进行临床试验,与检查点抑制联合使用或作为单一疗法。
MDCs和树突细胞激活双特异性抗体
CD40在包括APCs、其他MDCs和B细胞在内的多种细胞类型中表达,但也在广泛的恶性细胞上表达。单克隆激动性CD40抗体可以通过诱导APCs成熟和激活抗原特异性T细胞和其他免疫细胞来触发抗肿瘤效应,从而促进肿瘤特异性免疫反应,特别是通过启动细胞毒性T细胞。除了具有剂量限制毒性的激动性CD40抗体外,还开发了针对CD40和各种TAAs如CEACAM5、EpCAM或间皮素的双特异性抗体。与其他TNF超家族成员一样,受体聚集在受体激活中起着关键作用。将CD40激动性抗体与针对肿瘤靶向抗原的抗体结合在双特异性抗体中,允许共刺激活性定向到TME,从而提高安全性和有效性。例如,针对CD40和CEACAM5或EpCAM的四价双特异性抗体的概念验证表明,与单一CD40抗体相比,它们增强了T细胞交叉启动。针对间皮素和CD40的双特异性抗体(ABBV-428)在体外和体外模型中展示了增强的APC和T细胞激活,并且在I期试验中显示出可接受的安全性概况。为了在肿瘤内而不是外周选择性激活CD40,生成了FAP×CD40,一种包含两个CD40结合位点和一个FAP结合位点的双特异性抗体。该抗体提供了一个强烈的FAP依赖性CD40刺激信号,展示了良好的安全性概况以及肿瘤积聚和肿瘤内免疫激活,目前正在进行I期临床试验。MP-0317是一种多功能设计ankyrin重复蛋白(DARPin),应用相同的概念,针对FAP、CD40和HSA进行半衰期延长,目前正在进行I期临床研究。或者,双特异性抗体可以通过Clec12a标记物直接靶向树突细胞。
双特异性抗体的双重共刺激
在免疫细胞上双重靶向两种不同的共刺激受体已被用于诱导强大的抗肿瘤反应。FS120是一种针对活化T细胞上表达的4-1BB和OX40的四价双特异性抗体,以一种不依赖FcγR的方式激活CD4和CD8 T细胞。这种活性需要两个受体的共刺激才能有效激活免疫细胞并发挥抗肿瘤活性,支持使用四价双特异性抗体双重靶向共刺激受体以诱导有效的受体聚集和激活的概念。在动物研究中,FS120的替代品没有引起肝脏炎症和肝毒性,这是激动性4-1BB抗体观察到的限制。FS120目前正在进行I期临床试验。类似的方法中,开发了一种双价双特异性抗体,用于双重靶向4-1BB和CD40(BNT-312,tecaginlimab),因此靶向T细胞和APCs。APCs的CD40激活导致共刺激分子的上调和免疫刺激性细胞因子的分泌,从而在不依赖CD4 T细胞帮助的情况下,实现强大的CD8 T细胞介导的抗肿瘤免疫反应。
双特异性抗体用于双重检查点抑制和共刺激
抗共刺激受体的抗体还被与CPIs结合使用,以释放T细胞免受抑制信号的影响,同时增强T细胞反应,特别是在对检查点抑制有抵抗力或难治性的肿瘤中。大多数目前正在临床试验中的双特异性抗体使用跨作用的方式结合这些信号,通过靶向肿瘤细胞上的PDL1和免疫细胞上的共刺激受体,其中4-1BB是最突出的靶标。超过十种不同的针对PDL1和4-1BB的双特异性抗体正在进行I期或II期试验。II期候选物包括一种IgG-anticalin融合蛋白(PRS-344),其中配体结合anticalin框架代表第二特异性,一种双价双特异性IgG抗体(acasunlimab,也称为GEN1046)和一种三价,三特异性单链二抗体-scFv融合蛋白,进一步包含一个HSA结合位点以延长半衰期(NM21-1480)。这些类型的双特异性抗体可以增强免疫反应,超越单一抗体及其组合,进一步提供针对PDL1表达肿瘤细胞的靶向共刺激,以及TME中的MDCs和肿瘤引流淋巴结。与此一致,TME中表达4-1BB的肿瘤浸润CD8 T细胞亚群表达高水平的PD1,因此容易受到PDL1×4-1BB双特异性抗体的治疗。值得注意的是,由于4-1BB信号需要超聚集,与PDL1的结合可以导致TME中条件聚集和激活的4-1BB,减少肝脏毒性,如四价双特异性IgG-scFv(ABL503)所示。遵循这一概念的进一步双特异性抗体包括四价双特异性单克隆抗体(FS222)和双价双特异性IgGs,如MCLA-145。同样,CD28共刺激和检查点抑制可以通过在肿瘤内顺式作用的T细胞双重靶向进一步实现。ATOR-1015的可行性已得到证明,它是一种针对OX40的IgG,融合到针对CTLA4的优化版本的V型域的CD86上。与4-1BB类似,CTLA4和OX40在活化的T细胞上上调,并由Treg细胞表达,特别是在TME中。与GITR和ICOS不同,CD27由naive T细胞表达,因此有助于促进新的T细胞反应。
PDL1×CD27双特异性抗体在临床前研究中比PD1阻断和CD27共刺激的组合更有效,同时展现出良好的安全性概况。在概念上类似的方法中,PD1的结合位点与其他TNF超家族的共刺激成员结合,包括4-1BB(如与IBI319结合)、GITR和ICOS(XmAb23104)。GITR也在活化的T细胞上上调,并由Treg细胞恒定表达,在其中发挥着增强初始免疫反应的关键作用。PD1×GITR-L双特异性融合蛋白的概念验证已经展示。对于这些药物中的一些,与联合或分别协同效应相比,检查点抑制的相对贡献并不一定确立。
新兴概念
支持双特异性抗体开发的概念从早期探索性方法迅速发展到临床开发,双特异性抗体现在已确立为治疗原则。然而,双特异性抗体领域仍在不断进展,以进一步探索和扩展技术和应用。学术界以及生物技术和制药工业追求的各种早期探索性双特异性抗体方法是有希望的,其中一部分可能提供尚未由当前开发中的双特异性抗体解决的治疗概念。本综述的范围不允许我们涵盖所有或许多这样的早期方法,实际上在这个快速增长的领域中可能无法全面覆盖。因此,我们通过提及一些我们认为相关并有潜力进一步推动基于双特异性抗体的癌症治疗界限的新兴主题来结束我们的综述。
三特异性TCEs与集成共刺激
共刺激信号可以与双特异性TCEs结合,以促进有效的T细胞激活。这已经通过上述的双特异性TCEs和共刺激双特异性抗体的组合实现,但也通过在双特异性TCE中包含第三个结合位点来针对共刺激受体,从而生成三特异性抗体。目前有两种这样的三特异性TCE正在进行临床试验,它们针对TAA和CD3,并进一步包含一个针对CD28的结合位点。SAR443216是一种三价三特异性免疫球蛋白基抗体,针对HER2×CD3×CD28,包含一个突变的IgG4,缺乏Fc介导的效应功能。这种三特异性抗体目前正在I期临床试验中,能够激活初级CD4和CD8 T细胞,诱导T细胞增殖,释放细胞因子和颗粒酶B以及T细胞介导的HER2表达肿瘤细胞的杀伤,包括HER2表达低的细胞。类似地,一种针对在多发性骨髓瘤中过度表达的CD38的结合位点与CD3和CD28结合位点结合在三特异性抗体SAR442257中,目前也在I期临床试验中。
前药方法
一种新兴的方法旨在通过提供“安全关键”的特异性作为前药,在肿瘤处选择性激活,从而生成具有高度肿瘤特异性功能的双特异性抗体。一些应用于失活抗体以生成前药并在肿瘤处重新激活的概念如图4所示。前药转化为功能性双特异性抗体可以通过肿瘤微环境中存在的肿瘤特异性蛋白酶等环境触发因素来实现。例如,具有空间屏蔽的双特异性抗体可以通过蛋白酶激活。需要肿瘤特异性蛋白酶表达的蛋白酶激活TCEs,即所谓的probodies,需要肿瘤特异性蛋白酶在TME中的表达才能激活。另一种早期阶段的双重肿瘤靶向方法依赖于从两个具有分裂CD3ε结合基团的双特异性抗体中肿瘤特异性组装功能性CD3ε抗体片段。这些实体需要被设计为在循环中作为单独实体时不活跃,以便它们只在肿瘤抗原结合和随后的原位组装后被激活,如已经为半抗体或前药激活链交换(PACE)分子所描述的那样。这类分子面临的主要挑战仍然是以单体形式大规模生产它们,并防止在没有目标结合的情况下过早组装。通过目标链交换介导的分裂型I细胞因子的重建就是一个例子,说明如何实现肿瘤特异性组装。值得注意的是,最近开发了一种引入到抗4-1BB抗体结合位点的ATP依赖性开关,以增加肿瘤选择性并避免靶上、靶外毒性。这种开关使用肿瘤中升高的ATP水平作为触发因素,可能也适用于其他结合实体。
图4 | 双特异性抗体领域的新兴概念。a, 带有集成共刺激的三特异性T细胞招募剂(TCEs),用于通过CD3结合同时激活T细胞受体(TCR)(信号1)和通过结合CD28进行共刺激(信号2)。b, 双特异性抗体(bsAb)前药的作用方式。用于生成前药并重新激活所需作用位点的抗体的一般概念包括:阻断结合位点以使抗体失活,以及通过蛋白酶诱导激活被阻断的抗原结合位点,对目标环境(如酸性pH或ATP)的亲和性调节,以及由于通过高浓度局部富集互补前药而进行的组装或交换反应。c, 通过结合表面抗原(肿瘤相关抗原(TAA))和降解分子,例如膜E3连接酶,实现蛋白酶体靶向嵌合体(PROTAC)方法,这导致细胞表面目标的内化和蛋白酶体降解。d, 例如通过基因疗法将bsAb传递到CAR-T细胞中。e, 细胞因子模拟bsAb触发细胞因子受体途径,如通过将受体域引入立体接近性,模仿细胞因子作用的IL-2Rβ–IL-2Rγ异二聚体。
PROTAC双特异性抗体
另一个新兴概念和新的作用机制最近被描述,它使用双特异性抗体通过靶向降解来灭活与增殖相关的过程。类似于新兴的双特异性或多特异性小分子蛋白水解靶向嵌合体(PROTACs)领域,双特异性抗体可以被设计为触发内部化并随后降解参与癌症发展和/或进展的表面蛋白。这样的双特异性抗体同时结合到被靶向降解的蛋白质,以及触发结合目标蛋白的内部化和随后降解的因素,如膜可及的E3泛素连接酶或转铁蛋白受体。目前还没有已知的抗体-PROTAC概念进入临床研究,但这类实体的开发与“标准”双特异性抗体的开发完全兼容,并为靶向新途径并尽快将其概念带入临床提供了独特的可能性。
双特异性抗体的传递
双特异性抗体发展的另一个重要新兴概念是局部生产和随后的局部传递双特异性抗体,例如通过脂质纳米粒子介导的mRNA传递CLADN6 TCE,溶瘤病毒或类似基因疗法的方法,包括CAR-T细胞。
细胞因子模拟抗体
最后,双特异性抗体也可以作为细胞因子模拟物或所谓的合成细胞因子激动剂。在这种情况下,已经描述了scFvs或基于单一结构域Vhh的方法,通过模仿IL-2或IL-15、IL-18、I型干扰素和IL-10有效地触发细胞因子信号。或者,可以通过使用分裂方法使用新设计的IL-2模拟蛋白neoleukin实现肿瘤特异性细胞因子受体激动活性。这种基于抗体的细胞因子模拟物在癌症免疫疗法中可能有各种应用。
展望
双特异性抗体领域近年来取得了显著进展,到2023年底,已有十多种双特异性抗体获得批准,许多不同的方法正在临床测试中。然而,我们认为,由于癌症的异质性和适应性,这些方法中不太可能有一种成为通用的癌症免疫疗法。相反,抗体将需要为特定应用量身定制,并将依赖于与其他方法的结合,以最大化它们的疗效和安全窗口。具有多重特异性的抗体治疗的发展增长可能会在未来几个领域发生:针对具有明确依赖性的肿瘤的肿瘤相关RTKs的双特异性抗体;用于以增加的选择性靶向肿瘤的双特异性ADCs;用于靶向降解适用于各种途径的细胞表面蛋白的双特异性PROTACs;以及用于癌症免疫疗法的多特异性抗体。在后一个领域,特别是对于非常有效的基于T细胞的疗法,如TCEs或CAR-T细胞,识别高度肿瘤选择性抗原将是至关重要的,将需要能够通过肿瘤特异性蛋白酶激活和更好地调节效应功能来特别实现肿瘤特异性活性,同时保护正常组织。另一个重要方面是提供双重检查点抑制和/或补充共刺激信号给T细胞,以维持和延长T细胞反应,如已被证明对CAR-T细胞疗法的临床成功至关重要。重要的是,这种方法不仅适用于与TCEs的组合,也适用于与内源性免疫方法的组合。另一个重要方面是通过激活先天免疫系统,包括自然杀伤细胞、MDCs和树突细胞,促进二次免疫反应的产生。与其他癌症药物一样,通过改进的诊断方法和新的发展范式,使双特异性抗体和多特异性基于抗体的治疗能够在疾病早期应用于患者将是实现治愈癌症患者目标的关键。
免疫疗法引进/卖出抗体药物偶联物细胞疗法申请上市
2024-03-12
On March 6th, the journal Nature Reviews Drug Discovery published a review article discussing the latest advances and applications of bispecific antibodies (bsAbs) in cancer treatment.
Bispecific antibodies (bsAbs) offer a unique advantage due to their ability to target two different antigens simultaneously, which helps to enhance the immune system's recognition and killing of tumor cells. As of the end of 2023, 14 bsAbs have been approved: 11 for cancer treatment and 3 for non-oncological indications. BsAbs come in various structural formats, target different antigens, and mediate antitumor functions through different molecular mechanisms.
In the study, the authors outlined recent advances in the application of bsAbs in the field of cancer therapy, focusing on bsAbs that are either approved or in clinical development stage. This includes but is not limited to: bispecific antibody-mediated dual signaling pathway modulators, tumor-targeted receptor agonists, bsAb-drug conjugates, bispecific T cells, natural killer cells, and innate immune cell activators, as well as bispecific checkpoint inhibitors and co-stimulators.
Furthermore, the authors also envisioned next-generation bsAbs that are in early development stages, which include trispecific antibodies, bsAb prodrugs, bsAbs that induce tumor-target degradation, and bsAbs that mimic cytokine functions. These novel bsAbs hold the promise to further expand the range and strategies of cancer treatment, providing more precise and efficient therapeutic options.
Current Status of Bispecific Antibody ResearchOver the past decade, bispecific antibodies (bsAbs) have garnered significant attention due to their unique multimodal mechanisms of action. Between 2021 and 2023, nine bsAbs have been approved for cancer treatment, reflecting the development trajectory of such antibodies as novel therapeutic agents. The success of bsAbs lies in their ability to surpass the therapeutic effects of natural monospecific antibodies, for instance by recruiting immune effector cells to cancer cells, or by targeting different signaling pathways simultaneously with one molecule.
According to statistics, there are currently over 200 bsAbs in clinical development. Among these, 50% have entered Phase II or Phase III clinical trials, and some have already been approved for marketing. Approximately three-quarters of bsAbs are being developed for the treatment of solid tumors, and within the realm of solid tumor therapy, T cell engagers (TCEs, accounting for 32.9%) as well as bsAbs with checkpoint inhibition and/or immunomodulatory mechanisms (accounting for 45.1%) hold a dominant position.
In contrast, bsAbs targeting hematological malignancies are primarily composed of TCEs (accounting for 75%) and other mechanisms of immune activation (accounting for 21.9%). These mechanisms usually achieve checkpoint inhibition and/or immunomodulatory effects on natural killer cells and other immune cells through the exploitation of highly tumor-selective or lineage-specific antigens. Notably, around 10% of bsAbs for the treatment of solid tumors have adopted a dual signal inhibition strategy.
Below is an overview of the 11 bispecific antibodies approved for cancer treatment:
Catumaxomab (Removab): The first approved bispecific antibody (bsAb), developed in collaboration by Trion Pharma and Fresenius, targets EpCAM and CD3ε, and was used for the treatment of malignant ascites (such as that associated with ovarian cancer), but was withdrawn from the EU market in 2013.
Blinatumomab (Blincyto): Developed by Amgen, this bispecific T cell engager (TCE) targets CD19 and CD3ε with a BiTE 1+1 format. It was approved in 2014 in the United States, European Union, and Japan for the treatment of acute lymphoblastic leukemia (ALL).
Amivantamab (Rybrevant): Developed by J&J, this agent targets both EGFR and MET. Its mechanism of action includes signal transduction inhibition and antibody-dependent cellular cytotoxicity (ADCC) effects, using a Duobody 1+1 format. It was approved in the United States and European Union in 2021 for the treatment of non-small cell lung cancer (NSCLC) with EGFR exon 20 insertion mutations.
Tebentafusp (KIMMTRAK): Produced by Immunocore, this agent targets the gp100-HLA-A*02 complex and CD3ε. It is a TCE in the form of an scFv-TCR fusion protein. It was approved in 2022 in the United States and European Union for the treatment of uveal melanoma.
Mosunetuzumab (Lunsumio): Developed by Roche, this is a bispecific TCE that targets CD20 and CD3ε, using a KiH 1+1 IgG format. It was approved in 2022 in the United States and European Union for the treatment of relapsed/refractory follicular lymphoma.
Cadonilimab (Kaitanni): Developed by Akeso, a Chinese biopharmaceutical company, this agent targets PD1 and CTLA4 and is classified as a dual immune checkpoint inhibitor. It has an IgG-scFv tetrabody 2+2 structure and was approved in China in 2022 for the treatment of hepatocellular carcinoma.
Teclistamab: Also introduced by J&J, teclistamab is a bispecific T-cell engager (TCE) targeting BCMA and CD3ε. Utilizing a Duobody 1+1 structure, it was approved in 2022 in the United States and the European Union for the treatment of relapsed/refractory multiple myeloma.
Glofitamab (Columvi): Originating from the Roche Group, glofitamab is a CD20 and CD3ε bispecific TCE using a CrossMAb 2+1 structure. It received approval in 2023 in the United States and the European Union for the treatment of relapsed/refractory diffuse large B-cell lymphoma (DLBCL).
Epcoritamab (T)Epkinly: Jointly developed by Genmab and AbbVie, epcoritamab is also a TCE targeting CD20 and CD3ε. It features a Duobody 1+1 structure and was approved in 2023 in the United States, the European Union, and Japan for the treatment of relapsed/refractory DLBCL.
Talquetamab: Another product from J&J, talquetamab targets GPRC5D and CD3ε, and is also a TCE type. Using a Duobody 1+11 structure, it was approved in 2023 in the United States and the European Union for the treatment of relapsed/refractory multiple myeloma.
Elranatamab (Elrexfio): Developed by Pfizer, elranatamab targets BCMA and CD3ε as a TCE. With a bsAb (bispecific antibody) 1+1 structure, it was approved in 2023 in the United States and the European Union for the treatment of relapsed/refractory multiple myeloma.
The discovery of new bsAbs is primarily driven by the underlying biological principles, and it is necessary to match them with optimal bsAb designs in order to select the correct structural forms, affinity ranges, and epitopes. Characteristics such as target selection, epitope positioning, affinity, valency, distance between binding sites, molecular size, flexibility, and the presence of an Fc region and its mediated effector functions have profound impacts on the functional attributes and developmental feasibility.
Based on whether they engage T-cells, the marketed bsAbs can be categorized into T-cell engaging and non-T-cell engaging types.
T cell engager (TCE) category of bsAbs: The primary purpose of designing this class of antibodies is to connect T cells and tumor cells via specific antigen-binding sites, thereby activating the cytotoxic activity of T cells against tumor cells. Among the 11 approved bsAbs, 6 have structures similar to IgG, consisting of two heavy chains (with the constant region depicted in dark grey, VH domains in dark blue or dark red) and two light chains (constant region in light grey, VL domains in light blue or light red). Most of these bsAbs adopt a 1+1 ratio, meaning each antigen has one binding site; additionally, there is one TCE that utilizes a 2+1 ratio model by fusing an extra Fab fragment onto one heavy chain, allowing it to bind two different antigens simultaneously.
Non-T cell engager category of bispecific antibodies: These bsAbs include different types of constructions. For example, blinatumomab is an Fc-fragment lacking fusion protein composed of two single-chain variable fragments (scFv) stitched together; tebentafusp is a product where an scFv fragment is fused with a T cell receptor (TCR) fragment. There are also IgG-scFv fusion proteins with a 2+2 ratio mode, meaning they contain two full IgG domains and two scFv domains, capable of binding simultaneously to two different antigens.
Representative monoclonal antibodies in clinical research:
The mechanism of action of bsAbsBispecific antibodies (bsAbs) exhibit immense potential in cancer therapy due to their unique design and diverse mechanisms of action.
The following is a brief overview of the different mechanisms of bispecific antibodies and their underlying principles:
Dual receptor inhibitor bispecific antibodies: Bispecific antibodies with dual receptor-blocking capabilities can simultaneously target two different cell surface receptors, such as EGFR, HER2, and VEGF.
For instance, Amivantamab (JNJ-61186372) is a bispecific antibody designed to concurrently bind to the epidermal growth factor receptor (EGFR) and the hepatocyte growth factor receptor (MET). These receptors play key roles in the pathogenesis of non-small cell lung cancer (NSCLC), promoting the proliferation and survival of tumor cells. Traditional monospecific therapies may lead to resistance as tumor cells exploit alternative compensatory signaling pathways. However, as the first approved bispecific antibody targeting both receptor tyrosine kinases, Amivantamab can more effectively inhibit the progression of NSCLC. By simultaneously blocking both the EGFR and MET signaling pathways, it can reduce or overcome resistance due to redundancy associated with single-drug treatments.
The design purpose of zenocutuzumab (MCLA-128) is to simultaneously bind to both the HER2 and HER3 receptors. This dual-targeting strategy utilizes the biological characteristic of the interactions between members of the HER family: HER2 and HER3 are capable not only of forming homodimers but can also create heterodimers with other HER family members (including EGFR), activating downstream signaling pathways that promote tumor cell growth, survival, and metastasis. In clinical studies, zenocutuzumab has been found to have therapeutic potential in patients with solid tumors harboring NRG1 gene fusions. NRG1 is a ligand for HER3, and its binding to HER3 induces the formation of the HER2/HER3 heterodimer complex, thereby driving cancer cell proliferation. By simultaneously blocking HER2 and HER3, zenocutuzumab is anticipated to prevent the activation of this pro-tumorigenic signaling pathway, thereby inhibiting the progression of this specific type of tumor.
Ligand-Receptor Inhibitory bsAbs: Ligand-receptor inhibitory bispecific antibodies (bsAbs) block signal transduction by interfering with the binding of ligands to their receptors or by inhibiting receptor homodimerization. For example, bispecific antibodies targeting VEGF and ANG2 can simultaneously blockade the VEGFR and TIE2 pathways, both of which promote angiogenesis, thereby suppressing tumor growth and metastasis.
Vanucizumab is one such bsAb that concurrently inhibits the biological activities of two different biomolecules, VEGF-A and angiopoietin-2 (ANG2). VEGF and ANG2 are cytokines that play key roles in the genesis and progression of tumors by activating their respective receptor pathways to stimulate tumor neovascularization, which in turn supports tumor growth, invasion, and metastasis. In preclinical model studies, vanucizumab has demonstrated significant anti-tumor, anti-angiogenic, and anti-metastatic activities.
Similarly, BI836880 is a trispecific nanobody-based fusion protein comprising three distinct nanobodies that respectively target VEGF (Vascular Endothelial Growth Factor), ANG2 (Angiopoietin-2), and HSA (Human Serum Albumin). The design of this drug aims to inhibit tumor growth and spread by simultaneously blocking VEGF and ANG2, two key signaling pathways involved in tumor angiogenesis. The portion that binds to HSA is intended to extend the drug's half-life in the human body, ensuring a more prolonged therapeutic effect.
Receptor-Activated bsAbs: Activating bi-specific antibodies (bsAbs) function by promoting the formation of effective clusters of specific receptors to activate their downstream signaling pathways, such as targeting the members of the TNFRSF family and their receptors.
For example, RO6874813 (also known as RG7386) is a tetravalent bi-specific antibody designed to target cancer-associated fibroblasts (CAFs) surface Fibroblast Activation Protein-alpha (FAPα) and Death Receptor 5 (DR5). FAPα is highly expressed in the Tumor MicroEnvironment (TME), particularly on CAFs associated with tumor progression and metastasis. DR5, a member of the TNF superfamily, can initiate apoptosis in cancer cells when activated by a specific ligand like TRAIL. RO6874813, by binding to both FAPα and DR5, can efficiently direct pro-apoptotic signals to tumor cells and enhances the selectivity and potency toward DR5 by avoiding degradation or inactivation caused by endogenous or exogenous decoy receptors. In experimental studies, this drug has demonstrated strong selectivity and in vivo antitumor activity, effectively killing tumor cells in FAPα-positive mouse models, and therefore it has great potential as a novel anti-cancer therapy.
BsAbs for Directed Payload Delivery: BsAbs designed for targeted payload delivery typically employ two strategies: one is pretargeted therapy, which initially uses one binding site to deliver the drug to the tumor site, followed by the capture of a radiolabeled payload or drug complex with another site; the other involves directly linking toxins or radioactive isotopes to the bsAb to selectively kill cancer cells. For example, a bsAb targeting CEACAM5 or HER2 can carry a radioactive isotope, delivering it precisely to the tumor tissue.
For instance, zanidatamab zovodotin (ZW49) is a bispecific antibody-drug conjugate (bsADC) that combines a bispecific antibody targeting the HER2 receptor with a cytotoxic payload derived from Auristatin. Zanidatamab is the core component of this ADC, capable of binding different epitopes on the HER2 receptor concurrently. This biparatopic (dual-epitope targeting) mechanism helps to enhance the affinity for HER2-positive tumor cells and to form more stable and functionally potent HER2 complexes. ZW49 leverages this bispecific structure to precisely target cancers that express or amplify HER2, especially because once the auristatin-derived cytotoxin is conjugated, it can release its cytotoxic payload inside tumor cells upon entry, thereby exerting a cytotoxic effect and killing cancer cells.
Other Bispecific Antibodies (bsAbs) for Cancer Treatment: The mechanisms of action of most bispecific antibodies (bsAbs) used in cancer immunotherapy can be broadly classified into two categories. One category works by enhancing the natural or endogenous immune response driven by T cells, for example, by amplifying existing anti-tumor responses or overcoming immune checkpoint inhibition. The other category functions by providing synthetic immunity, such as through bsAb-mediated recruitment, activation, and interaction of immune cells. The article also overviews the most prominent mechanisms of action of bsAbs and multispecific antibodies, covering a variety of molecular design strategies including immune checkpoint inhibitors (CPIs), effector cell engagers, and co-stimulatory bsAbs.
Dual Checkpoint Inhibitors (Dual CPIs): In cancer immunotherapy, bispecific antibodies are used to block two different immune checkpoint proteins simultaneously, to more effectively relieve the suppression of T cell activity by tumors. For instance, designed bsAbs can target checkpoints like PD-L1 and CTLA4 at the same time.
Effector Cell Engagers: These bsAbs are designed to directly connect tumor cells to immune effector cells, such as natural killer cells (NK cells), macrophages, and dendritic cells (DCs), to promote the recognition and elimination of tumor cells by effector cells. For example, some bsAbs can bind to receptors such as NKp46 or NKp30 alongside tumor-associated antigens, thereby enhancing the NK cells' cytotoxic action against tumors; others operate by targeting CD3 molecules to engage T cells with tumor cells expressing specific antigens, like BiTEs and T-cell engagers.
Co-stimulatory bsAbs: These bispecific antibodies are designed to simultaneously activate two co-stimulatory receptors in the immune system to enhance the immune response. For instance, FS120 is a tetravalent bsAb targeting 4-1BB and OX40, which can effectively activate T cells and generate anti-tumor activity, while avoiding the hepatic toxicity issues possibly caused by agonistic 4-1BB monoclonal antibodies alone. Additionally, there is a bivalent bsAb targeting 4-1BB and CD40 (tecaginlimab), which not only activates T cells but also induces a robust CD8+ T cell-mediated immune response by activating dendritic cells (DCs).
MDCs and Dendritic Cell-Activating bsAbs: Some bsAbs are designed to specifically bind to markers on the surface of myeloid dendritic cells (MDCs) or DCs, such as Clec12a, for the precise delivery of immune activation signals. They activate DCs and improve their antigen-presenting capabilities, thereby triggering a potent CD8+ T cell immune response.
Tumor-Targeting Co-stimulatory bsAbs: These antibodies are engineered to target specific antigens on tumor cells while activating co-stimulatory receptors of the immune system. For instance, bsAbs against CD47 can block the "don't eat me" signal, making tumor cells more susceptible to recognition and clearance by phagocytic cells. In addition, they can recruit other effector cells through the Fc region, increasing the aggressiveness towards the tumor.
Innate Immune Cell Engagers and T Cell Engagers: These bispecific antibodies (bsAbs) are designed to activate and direct natural killer (NK) cells and T cells to tumor cells. Some of these bsAbs retain or enhance the binding ability to FcγRIII to ensure the effective participation of NK cells; while others incorporate cytokines such as IL-2 or IL-15 into the bsAb structure to expand and activate the innate immune cell population.
PROTAC bispecific antibodies (bsAbs): This is a molecular drug that combines the technology of proteasome-mediated protein degradation with traditional bispecific antibody design strategies. These antibodies promote the tagging of target tumor-associated proteins with ubiquitin by simultaneously binding to E3 ubiquitin ligases or other factors capable of triggering internalization and subsequent degradation processes (such as membrane-accessible E3 ubiquitin ligases or transferrin receptors), leading to their degradation in the proteasome. Compared to traditional antibody therapies that only block signaling pathways to inhibit tumor cell growth, PROTAC bsAbs achieve a more thorough intervention by degrading target proteins, effectively addressing treatment failure due to drug resistance. Although this field is still in the early stages of development and no PROTAC bsAb has entered the clinical research phase, their design concept is compatible with the development of "standard" bispecific antibodies and provides a unique possibility for exploring new anti-cancer approaches. In the future, with further research and technological development, PROTAC bsAbs are expected to become a potent, highly selective, and targeted cancer treatment method.
Moreover, the article provides a detailed description of the design features of different bispecific antibody (bsAb) structures, such as using an IgG-like structure and ensuring the correct assembly of heavy chains and light chains through techniques like the "knobs-into-holes" technology and Fab-arm exchange (cFAE). It also discusses engineering modifications to the Fc region to attenuate or eliminate the binding to Fcγ receptors and complement, hence reducing nonspecific effects. The article also introduces the use of bsAbs to stimulate members of the TNFRSF family (e.g., DR4 and DR5) as potent and tumor-selective agonists. By designing bispecific antibodies that target tumor-associated antigens and TNFRSF members, efficient anti-tumor effects are achieved. It is noted that this mechanism is also applicable to costimulatory molecules that depend on receptor clustering for activation, such as 4-1BB, OX40, and CD40.
2023-07-06
·药研网
7月5日,中生制药子公司F-star宣布于武田达成合作协议,利用F-star的Fcab及mAb2技术平台,开发新一代多特异性免疫疗法,武田支付一笔未披露金额的预付款,约10亿美元里程碑金额,以及一定比例的销售分成。3月9日,中生制药发布公告,正式完成对F-star 收购事项,收购价格 1.61 亿美元。F-star主要技术是其专有的下一代四价 (2+2) 双特异性抗体平台,基于四价双抗平台,F-star已达成了数十项临床前及临床项目合作,主要合作方默克、强生及阿斯利康等。该平台是在天然抗体的Fc区创建两个不同抗原结合位点,称为 Fcab。产生的四价 (2+2) mAb2 双特异性抗体同时结合两种不同的抗原,通过crosslinking,clustering和conditionality三种方式实现安全、有效的免疫激活。Crosslinking:将两个不同的细胞或同一细胞上的两个受体结合起来,以激活免疫系统;Clustering:将受体聚集在细胞表面,以激活关键的免疫细胞途径;Conditionality:只有当受体同时被双抗结合时,免疫细胞才会被激活,保证安全性。生成的四价mAb2双抗是天然全人源抗体,引入Fcab抗原结合位点不会干扰与Fc受体的结合。可以将突变引入Fcγ受体结合位点,以提供最佳的免疫激活,并具有理想的安全性。同时也具有其他技术形式创造的潜力,如三特异性和Fc融合蛋白。目前临床资产中有三项是基于该平台创造的,三项资产以PD-(L)1为中心,用于PD-1耐药、PD-1联用和PD-L1低表达肿瘤患者。FS118(LAG-3/PD-L1双重抑制剂)FS118通过双特异性活性驱动PD-L1依赖性的LAG-3脱落和受体下调,可能为患者提供更持久反应LAG-3脱落是克服和避免PD-1耐药的一个重要机制,FS118可用于CPI耐药和CPI无效患者。在临床前研究中,FS118的抗肿瘤活性要优于单抗和单抗组合疗法。使用单剂量FS118后,可溶性LAG-3的呈剂量依赖性增加。LAG-3的脱落依赖于金属蛋白酶ADAM10和ADAM17。此前1期在PD-1耐药人群中的治疗数据显示,FS118耐受性良好,在20mg/kg以下的所有剂量水平上都没有出现DLT,治疗时间达79周。RP2D确认为10mg/kg QW。药效学活性延长,在整个用药期间可溶性LAG-3的水平持续上升,免疫细胞数量增加。所有患者中DCR为47%。在共表达LAG-3和PD-L1的肿瘤患者中观察到临床获益,其中一项间变性甲状腺癌(ATC)案例中,患者持续的临床获益达2年9个月。FS120(OX40/CD137双重激动剂)FS120 通过 FcgR 非依赖性机制同时结合到两个靶标来激活 CD4 和 CD8 T 细胞。FS120可用于与PD-1或化疗的联用中,协调PD-1,进一步激活免疫细胞,提高抗肿瘤疗效。体外研究中,FS120能够增强K药活性。在PD-1单抗难治性肿瘤模型中,联合治疗可显著提高生存获益。同时,联用下PD-1可降低FS120抗肿瘤活性阈值。FS120能够增强PD-1介导的细胞毒作用。联用可诱发强烈且短暂的促炎反应。目前,FS120正在接受一项1期单剂量递增试验,旨在确定FS120的安全、耐受性和药理活性剂量,确定后会启动与KEYTRUDA的联用治疗研究。FS222(PD-L1抑制剂/CD137激动剂)FS222主要针对PD-L1低水平表达的患者,通过阻断PD-1/PD-L1通路的同时,刺激CD137通路,促进免疫激活。最新公布的I期临床数据中,截止有33名患者接受了FS222的治疗,患者此前治疗方案中位数2种,其中25名患者CPI无效,剂量水平1mg/kg。最大耐受剂量尚未达到,安全性可控,大多数AEs为1-2级。一名患者出现了3级发热性中性粒细胞减少的DLT。8周后,1名患者出现CR,6名患者SD,16名患者PD(RECIST 1.1)。CR发生在一名PD-L1无效的PD-L1低表达非鳞状NSCLC患者身上,剂量1mg/kg。截至2022年7月20日,CR已持续了40.9周。据智慧芽数据库统计,PD-(L)1靶向药目前全球有五百多款药在研,多处于临床前和临床I期,其中中国在研数量最多。在该靶点如此火热的情况下,F-star纵向布局上,有PD-1耐药产品,横向布局上,有PD-1联用产品,加上PD-1低表达产品,F-star完美避开了激烈的竞争。细胞系产品查询投稿丨商务合作加入交流群往期推荐中生制药企业梳理PD1+ADC开卷:信达与荣昌达成合作完整版:2023 H1 药企裁员汇总点击下方“药研网”,关注更多精彩内容
并购免疫疗法
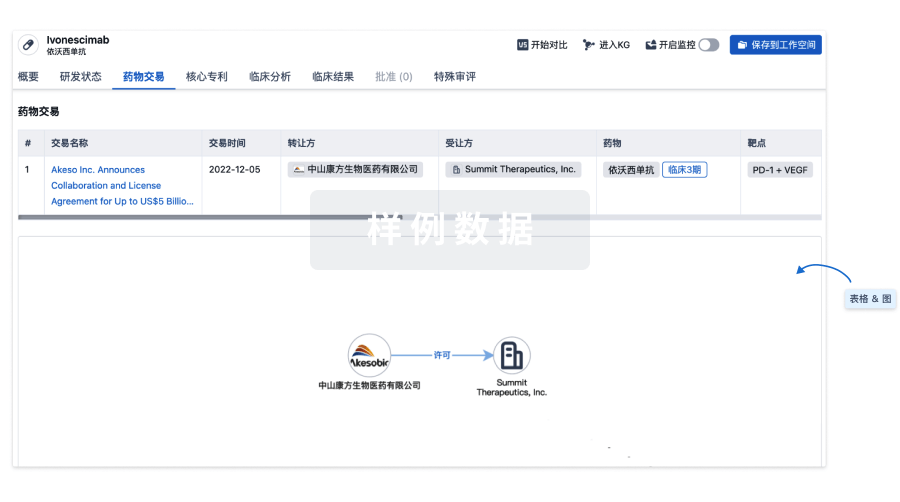
100 项与 FS-120 相关的药物交易
登录后查看更多信息
研发状态
10 条进展最快的记录, 后查看更多信息
登录
| 适应症 | 最高研发状态 | 国家/地区 | 公司 | 日期 |
|---|---|---|---|---|
| 肿瘤 | 临床1期 | 美国 | 2020-12-12 | |
| 晚期癌症 | 临床1期 | 美国 | 2020-11-18 | |
| 晚期癌症 | 临床1期 | 西班牙 | 2020-11-18 | |
| 肿瘤转移 | 临床1期 | 美国 | 2020-11-18 | |
| 肿瘤转移 | 临床1期 | 西班牙 | 2020-11-18 |
登录后查看更多信息
临床结果
临床结果
适应症
分期
评价
查看全部结果
| 研究 | 分期 | 人群特征 | 评价人数 | 分组 | 结果 | 评价 | 发布日期 |
|---|
No Data | |||||||
登录后查看更多信息
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
核心专利
使用我们的核心专利数据促进您的研究。
登录
或
临床分析
紧跟全球注册中心的最新临床试验。
登录
或
批准
利用最新的监管批准信息加速您的研究。
登录
或

生物类似药
生物类似药在不同国家/地区的竞争态势。请注意临床1/2期并入临床2期,临床2/3期并入临床3期
登录
或

特殊审评
只需点击几下即可了解关键药物信息。
登录
或

Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用


