预约演示
更新于:2025-05-07
Mycobacterium tuberculosis derived antigens(Vakzine)
更新于:2025-05-07
概要
基本信息
药物类型 重组蛋白 |
别名 rdESAT-6 / rCFP-10、Cy-Tb、Siiltibcy |
作用方式 调节剂 |
作用机制 结核分枝杆菌早期分泌性抗原调节剂 |
治疗领域 |
在研适应症 |
非在研适应症- |
非在研机构- |
权益机构- |
最高研发阶段批准上市 |
首次获批日期 欧盟 (2025-01-13), |
最高研发阶段(中国)- |
特殊审评- |
登录后查看时间轴
关联
100 项与 Mycobacterium tuberculosis derived antigens(Vakzine) 相关的临床结果
登录后查看更多信息
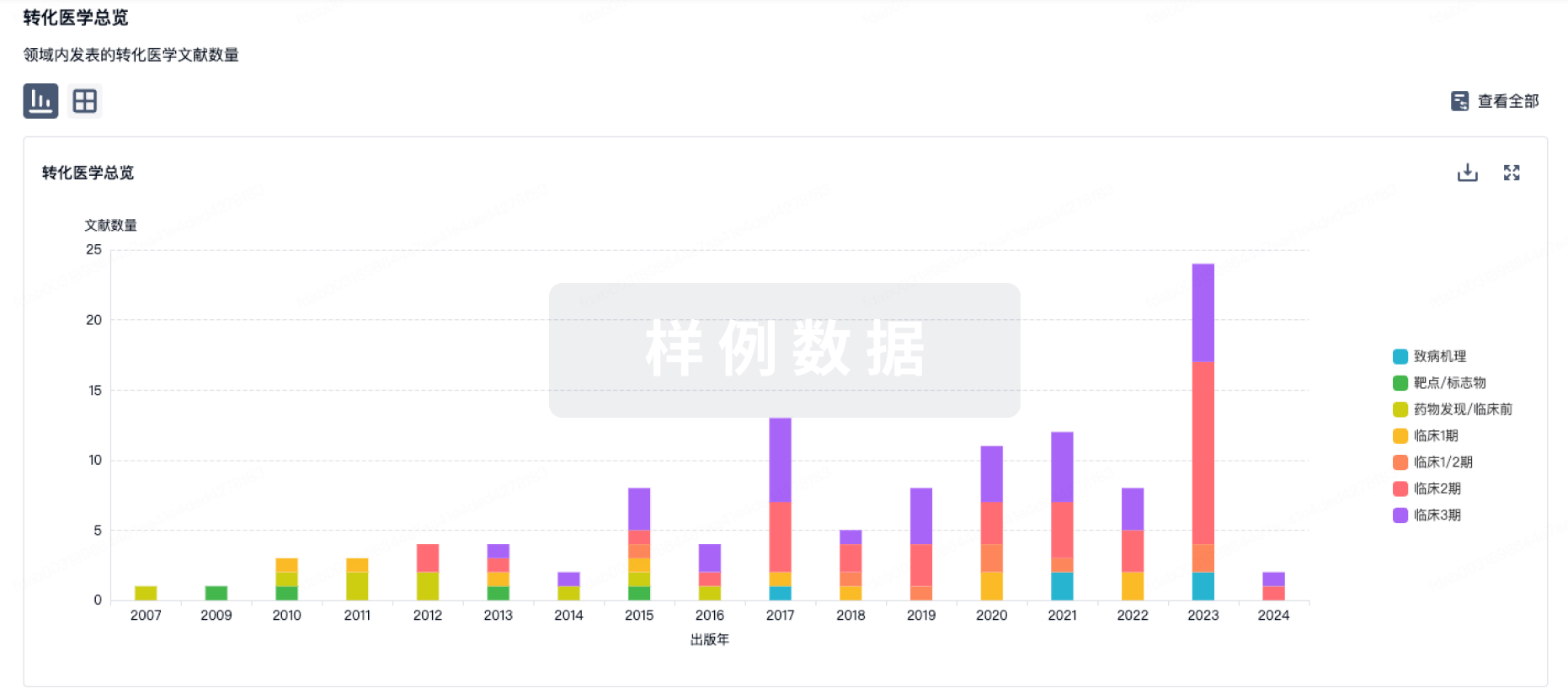
100 项与 Mycobacterium tuberculosis derived antigens(Vakzine) 相关的转化医学
登录后查看更多信息
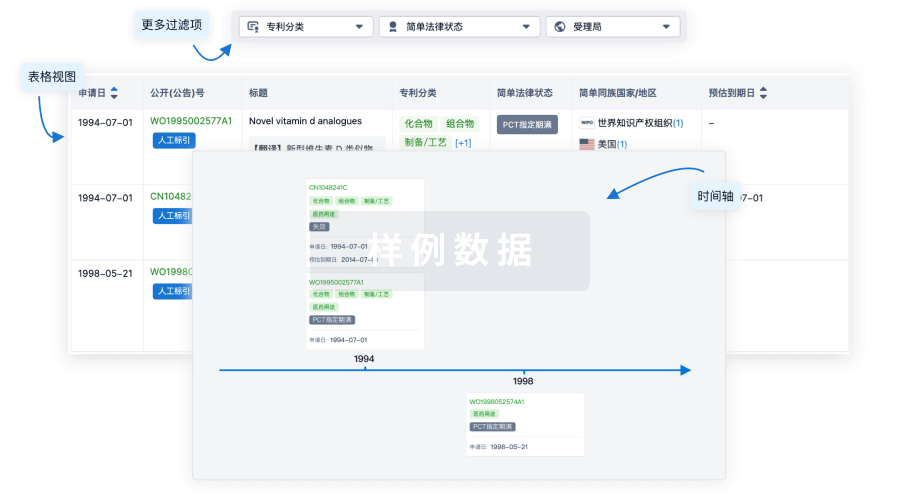
100 项与 Mycobacterium tuberculosis derived antigens(Vakzine) 相关的专利(医药)
登录后查看更多信息
3
项与 Mycobacterium tuberculosis derived antigens(Vakzine) 相关的文献(医药)2023-05-01·Open forum infectious diseases
A Systematic Review on the Safety of Mycobacterium tuberculosis-Specific Antigen-Based Skin Tests for Tuberculosis Infection Compared With Tuberculin Skin Tests.
Article
作者: Hamada, Yohhei ; Denkinger, Claudia M ; Ismail, Nazir ; Matveev, Aleksandr ; Korobitsyn, Alexei ; Abubakar, Ibrahim ; Ziganshina, Liliya Eugenevna ; Wang, Ting Ting ; Surkova, Elena ; Kontsevaya, Irina ; Wan-Hsin, Liu ; Rangaka, Molebogeng X
Cadernos de Saúde Pública
Testes cutâneos baseados em antígenos de tuberculose e QFT-Plus para diagnóstico da infecção por Mycobacterium tuberculosis em profissionais de saúde brasileiros: uma análise de custo-efetividade
Article
作者: Prado, Thiago Nascimento do ; Maciel, Ethel Leonor Noia ; Souza, Fernanda Mattos de ; Steffen, Ricardo E ; Pinto, Márcia Ferreira Teixeira ; Trajman, Anete
International Health
Evaluating the cost-effectiveness of Cy-Tb for LTBI in India: a comprehensive economic modelling analysis
Article
作者: Muniyandi, Malaisamy ; Rajsekar, Kavitha ; Padmapriyadarsini, Chandrasekaran ; Nagarajan, Karikalan ; Mathiyazhagan, Kavi ; Tyagi, Kirti
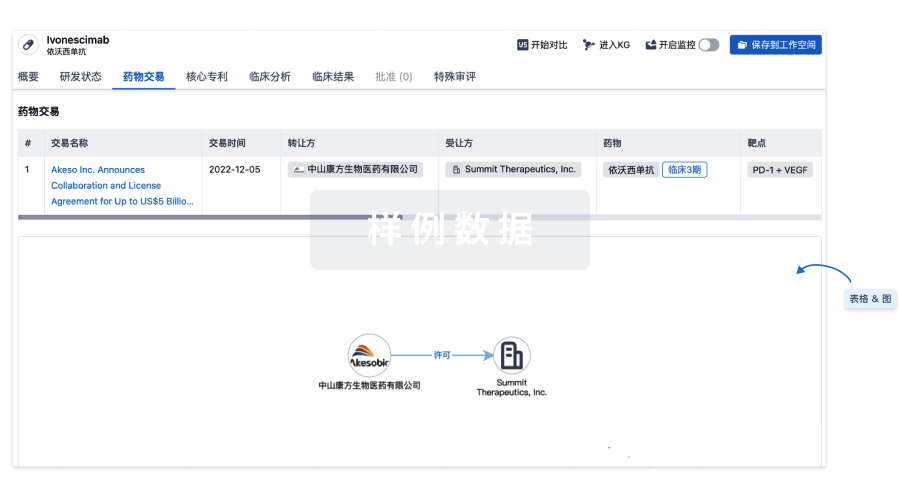
100 项与 Mycobacterium tuberculosis derived antigens(Vakzine) 相关的药物交易
登录后查看更多信息
研发状态
10 条最早获批的记录, 后查看更多信息
登录
| 适应症 | 国家/地区 | 公司 | 日期 |
|---|---|---|---|
| 结核 | 印度 | - |
登录后查看更多信息
临床结果
临床结果
适应症
分期
评价
查看全部结果
| 研究 | 分期 | 人群特征 | 评价人数 | 分组 | 结果 | 评价 | 发布日期 |
|---|
No Data | |||||||
登录后查看更多信息
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
核心专利
使用我们的核心专利数据促进您的研究。
登录
或
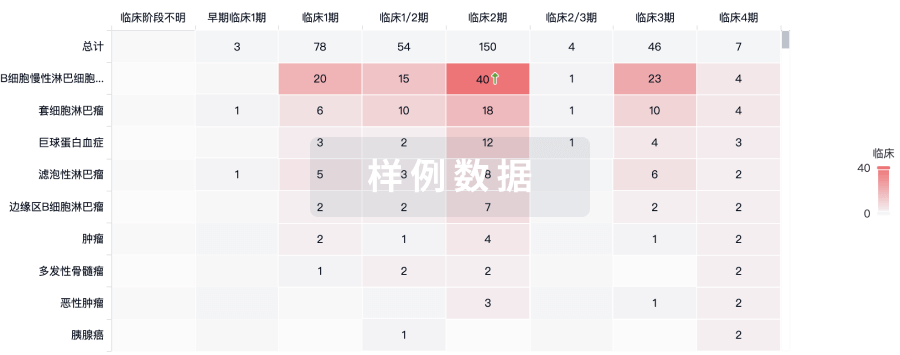
临床分析
紧跟全球注册中心的最新临床试验。
登录
或
批准
利用最新的监管批准信息加速您的研究。
登录
或

生物类似药
生物类似药在不同国家/地区的竞争态势。请注意临床1/2期并入临床2期,临床2/3期并入临床3期
登录
或

特殊审评
只需点击几下即可了解关键药物信息。
登录
或

Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用

