预约演示
更新于:2025-05-07
Amotosalen Hydrochloride
更新于:2025-05-07
概要
基本信息
药物类型 小分子化药 |
别名 |
靶点- |
作用方式- |
作用机制- |
治疗领域- |
在研适应症- |
非在研适应症- |
原研机构 |
在研机构 |
非在研机构- |
权益机构- |
最高研发阶段药物发现 |
首次获批日期- |
最高研发阶段(中国)- |
特殊审评- |
结构/序列
分子式C17H20ClNO4 |
InChIKeyMHLAMQBABOJZQW-UHFFFAOYSA-N |
CAS号161262-45-9 |
关联
100 项与 Amotosalen Hydrochloride 相关的临床结果
登录后查看更多信息
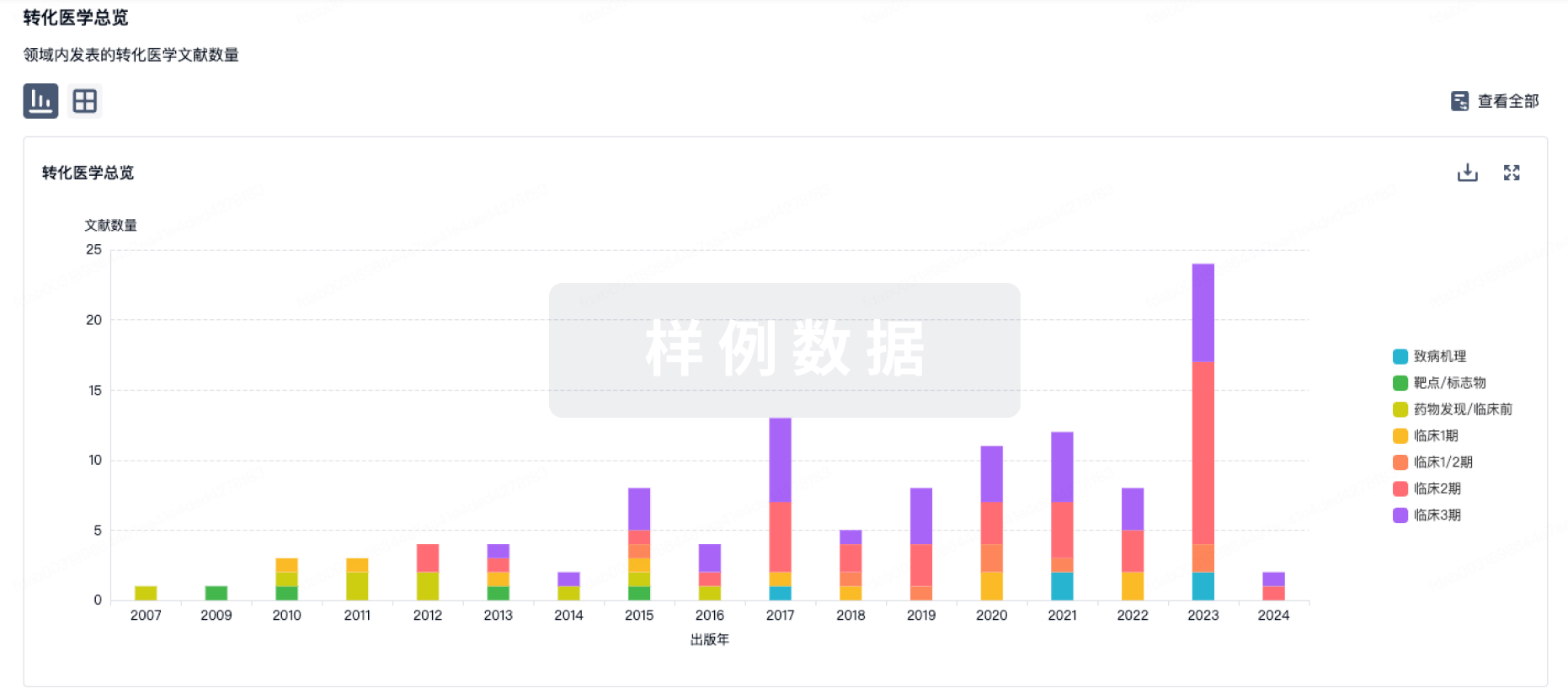
100 项与 Amotosalen Hydrochloride 相关的转化医学
登录后查看更多信息
100 项与 Amotosalen Hydrochloride 相关的专利(医药)
登录后查看更多信息
193
项与 Amotosalen Hydrochloride 相关的文献(医药)2025-02-01·Transfusion
Biotinylation of human platelets is compatible with pathogen inactivation treatment and cold storage for clinical studies
Article
作者: Martin, Agathe ; Prudent, Michel ; Alberio, Lorenzo ; Crettaz, David ; Aliotta, Alessandro ; Bertaggia Calderara, Debora ; Muret, Charlotte
2025-02-01·Current Stem Cell Research & Therapy
The Impact of Amotosalen Photochemical Pathogen Inactivation on Human Platelet Lysate
Article
作者: Vandewalle, Vicky ; Compernolle, Veerle ; Feys, Hendrik B. ; De Prest, Marie-Laurence ; Delabie, Willem ; Vandekerckhove, Philippe ; De Bleser, Dominique
2025-01-01·Transfusion
Effect of concurrent pathogen reduction (amotosalen/UVA ) and gamma/x‐ray irradiation on biochemical characteristics of apheresis platelets in additive solution
Article
作者: Vostal, Jaroslav G. ; Khoshi, M. Reza ; Skripchenko, Andrey ; West‐Mitchell, K. ; Seifu, Robel ; Villa, Carlos H. ; Simak, Jan ; Byrne, Karen ; Conry‐Cantilena, Cathy
1
项与 Amotosalen Hydrochloride 相关的新闻(医药)2024-04-06
血液制品(Blood Products)指源自人类血液或血浆的治疗产品,如人血白蛋白、人免疫球蛋白和人凝血因子等,是由健康人的血浆或特异免疫人血浆分离、提纯制成的治疗产品,用于诊断、治疗或被动免疫预防。血液制品的发展历程011900-1902年人类发现了ABO 血型系统。021914年开始使用枸橼酸钠和葡萄糖作抗凝剂,从而临床上实现了常规输血,但是全血不易大量储备和运输,其有效组分也未得到分离使用。03第二次世界大战第二次世界大战期间,美军在海外作战,急需运输、贮存和使用方便的"血浆代用品"抢救伤员,美国哈佛大学E.J Cohn教授与他的研究组在1941年建立了低温乙醇血浆蛋白分段分离法(简称Cohn法),制出了白蛋白并进行了临床观察,1942年Cutter等药厂用 Cohn 法大量生产白蛋白供应美军。041942-1943年期间免疫球蛋白、纤维蛋白原制剂、抗血友病球蛋白(即现在的人凝血因子VIII)以及凝血酶原复合物也相继投产,自此拉开了白蛋白及其他血浆蛋白组分的生产新纪元。051946年Cohn 教授领衔发表了人血白蛋白制备工艺,即经典的 Cohn 6 法。061949年E.J.Cohn教授又研制成功了用于分离制备丙种球蛋白的Cohn 9法。Cohn6+ 9法形成了工业化生产血液制品的完整体系,之后的数十年被美洲大多数血制制品生产单位采用。071962年苏黎世大学有机化学副教授Nitschmann与瑞士红十字会输血服务中心Kistler教授发明了一种对Cohn6+9法进行大胆改造的方法,有效地缩短了生产、提高了产量,这即所谓的Nitschmann-Kistler法,这种革新的方法随后被欧洲的血液制品生产厂家所使用。0820世纪50年代20世纪50年代出现的硫酸铵盐析法和利凡诺沉淀法用于从胎盘血中提取白蛋白和免疫球蛋白,由于原料短缺和稳定性不足等问题逐渐从大规模生产中退出。0920世纪60年代20世纪60年代逐步发展起来的凝胶过滤(分子筛层析)、离子交换层析、亲和层析等层析法成为各类活性蛋白成分、微量蛋白成分的主要分离方法。1020世纪70年代随着凝胶过滤、离子交换层析、亲和层析技术的发展,层析法被越来越多的应用于血液制品的生产。虽然至今还不能作为血液制品生产的主要工艺,但层析法和低温乙醇法的联合使用已在多种血液制品的生产中发挥着重要的作用。1120世纪80年代基因工程技术取得了前所未有的进展,开始出现了以基因工程技术制备的重组血浆蛋白制品,临床上具有和人源性血浆蛋白制品相似的治疗作用。👇随着血液制品种类日益丰富,生产工艺日趋复杂,使用环境不断变化,加强血液制品管理,保证血液制品的质量就显得愈加重要。由于血液制品的生产原料直接来源于人体,通过血浆和纯化血浆制品传播血源性病毒仍然被认为对使用者构成风险。因此,血液制品病毒安全性控制尤为重要。2002年至今,指导我国血液制品病毒去除/灭活工作的主要依据为《血液制品去除/灭活病毒技术方法及验证指导原则》(国药监注[2002]160号)(以下简称《指导原则》)。去除/灭活病毒方法的选择1 《指导原则》中对不同类血液制品选择的去除/灭活病毒方法侧重点提出大致要求。由于不同类血液制品潜在的污染病毒的可能性不同,为此选择病毒去除/灭活方法的侧重点也应有所不同:01凝血因子类制品生产过程中应有特定的能去除/灭活脂包膜和非脂包膜病毒的方法,可采用一种或多种方法联合去除/灭活病毒。02免疫球蛋白类制品对于免疫球蛋白类制品(包括静脉注射用人免疫球蛋白、人免疫球蛋白和特异性人免疫球蛋白)生产过程中应有特定的灭活脂包膜病毒方法。但从进一步提高这类制品安全性考虑,提倡生产过程中加入特定的针对非脂包膜病毒的去除/灭活方法。03白蛋白采用低温乙醇生产工艺和特定的去除/灭活病毒方法,如巴斯德消毒法等。常用去除/灭活病毒的方法2《指导原则》中主要提供了5种常用的灭活/去除病毒方法,包括巴氏消毒法、干热法、有机溶剂/去污剂处理法、膜过滤法和低pH孵放法等,并对每种方法的参数、技术要点有明确要求,具体见表1。 其中,膜过滤法是《指导原则》中唯一的病毒去除的方法,该方法的主要作用机制是粒径排阻分子筛和吸附。在生产过程中企业常采用35~50 nm孔径的膜去除病毒,随着制品生产过程中纯化水平的提高,目前15~20 nm孔径的膜也常有应用。该方法可去除大部分病毒,尤其对细小病毒B19可有效去除。该方法可串联、针对性强、下游污染少、蛋白回收率高,便于整合到工艺过程的多个工段。但由于过滤器滤膜只能一次性使用,成本较高。随着人们对滤膜研究的深入了解,不同滤膜生产企业的滤膜性能存在差异,预过滤层和精密截留层应考虑不同品牌滤膜和不同批次过滤器滤膜性能的一致性和适用性。《WHO指南》中对公认的病毒去除/灭活方法进行了比较详尽的综述,分为病毒灭活和病毒去除两部分,并在病毒灭活方法部分增加蒸汽加热法,在病毒去除方法部分增加沉淀法和色谱法,并对每种方法在优点、注意事项和需记录的关键参数方面进行了详细汇总。见表2、表3。研发中的新型去除/灭活病毒方法 随着科学技术的进步,一些新的去除/灭活病毒技术也在血液制品生产中有所应用,例如采用补骨脂素S-59 联合使用A波段紫外线(Ultra-violet A,UVA)处理,可灭活血浆中的病毒;254 nm波长紫外照射(Ultra-violet C,UVC)在人血白蛋白和人免疫球蛋白灭活病毒中的应用;60Coγ射线辐照;碘浓度为1.05 mg·mL-1的淀粉结合碘导致模型脂质包膜和非包膜病毒失活7 logs以上等方法。在许多情况下,这些方法几乎没有临床验证,故在实际血液制品生产中的使用意义不大。因此,我国《指导原则》中未具体提及这些方法。参考资料:1国家药品监督管理局法规网2徐宏山,岳广智,杨立宏等.我国与WHO血液制品去除/灭活病毒技术方法与验证指导原则的比较研究[J].中国药事,2023,37(04):367-375.识别微信二维码,添加生物制品圈小编,符合条件者即可加入生物制品微信群!请注明:姓名+研究方向!版权声明本公众号所有转载文章系出于传递更多信息之目的,且明确注明来源和作者,不希望被转载的媒体或个人可与我们联系(cbplib@163.com),我们将立即进行删除处理。所有文章仅代表作者观点,不代表本站立场。
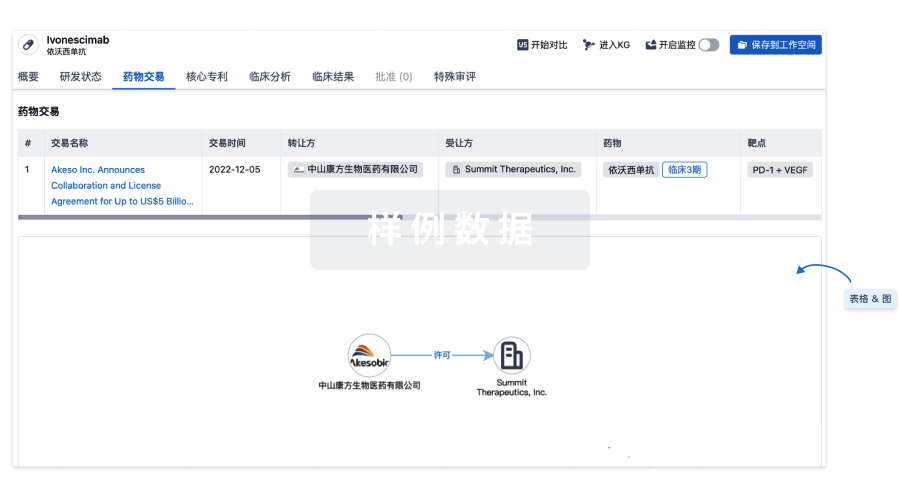
100 项与 Amotosalen Hydrochloride 相关的药物交易
登录后查看更多信息
研发状态
登录后查看更多信息
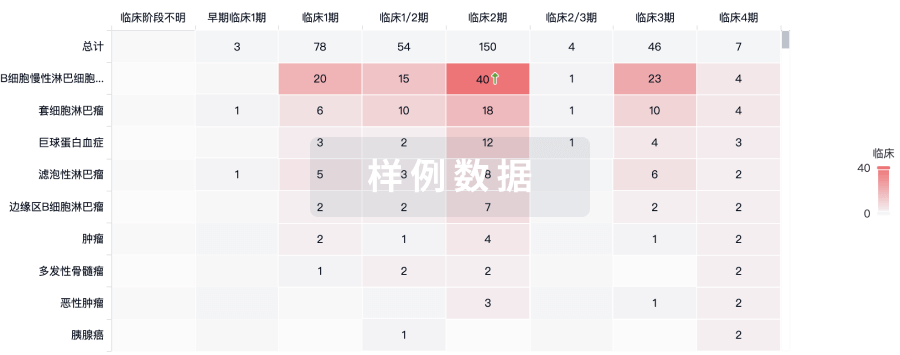
临床结果
临床结果
适应症
分期
评价
查看全部结果
| 研究 | 分期 | 人群特征 | 评价人数 | 分组 | 结果 | 评价 | 发布日期 |
|---|
No Data | |||||||
登录后查看更多信息
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
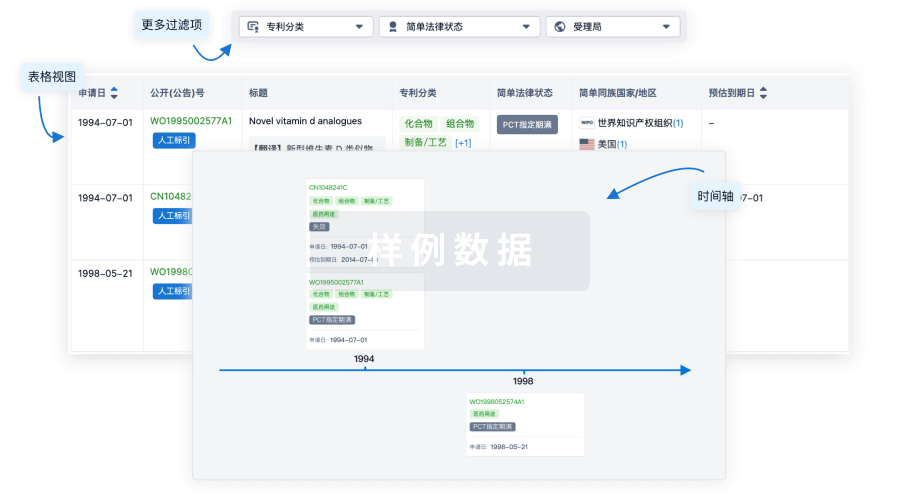
核心专利
使用我们的核心专利数据促进您的研究。
登录
或
临床分析
紧跟全球注册中心的最新临床试验。
登录
或
批准
利用最新的监管批准信息加速您的研究。
登录
或

特殊审评
只需点击几下即可了解关键药物信息。
登录
或

Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用
