预约演示
更新于:2025-05-24
CD7 CAR-T(Guangzhou Bio-gene Technology)
更新于:2025-05-24
概要
基本信息
药物类型 通用型CAR-T |
别名- |
靶点 |
作用方式 抑制剂 |
作用机制 CD7抑制剂(T细胞抗原CD7抑制剂)、免疫细胞毒性、T淋巴细胞替代物 |
非在研适应症- |
原研机构 |
在研机构 |
非在研机构- |
权益机构- |
最高研发阶段临床1/2期 |
首次获批日期- |
最高研发阶段(中国)临床1/2期 |
特殊审评- |
登录后查看时间轴
关联
2
项与 CD7 CAR-T(Guangzhou Bio-gene Technology) 相关的临床试验NCT05909527
A Single-arm, Open-label, Single-center Clinical Study: Safety and Efficacy of Anti-CD7 CAR-T in the Treatment of Relapsed or Refractory T Cell Lymphoblastic Acute Leukemia/ Lymphoma
This study is a single arm, non blind, randomized, single center study aimed at evaluating the safety, pharmacokinetic characteristics, and preliminary efficacy of CD7 CAR-T cell injection in r/r T-ALL/LBL subjects.
开始日期2023-05-01 |
申办/合作机构 |
ChiCTR2200062713
To evaluate the safety and efficacy of CLL1 /CD33/CD38/CD7 CAR-T in the treatment of relapsed and refractory acute myeloid leukemia
开始日期2022-08-17 |
申办/合作机构 |
100 项与 CD7 CAR-T(Guangzhou Bio-gene Technology) 相关的临床结果
登录后查看更多信息
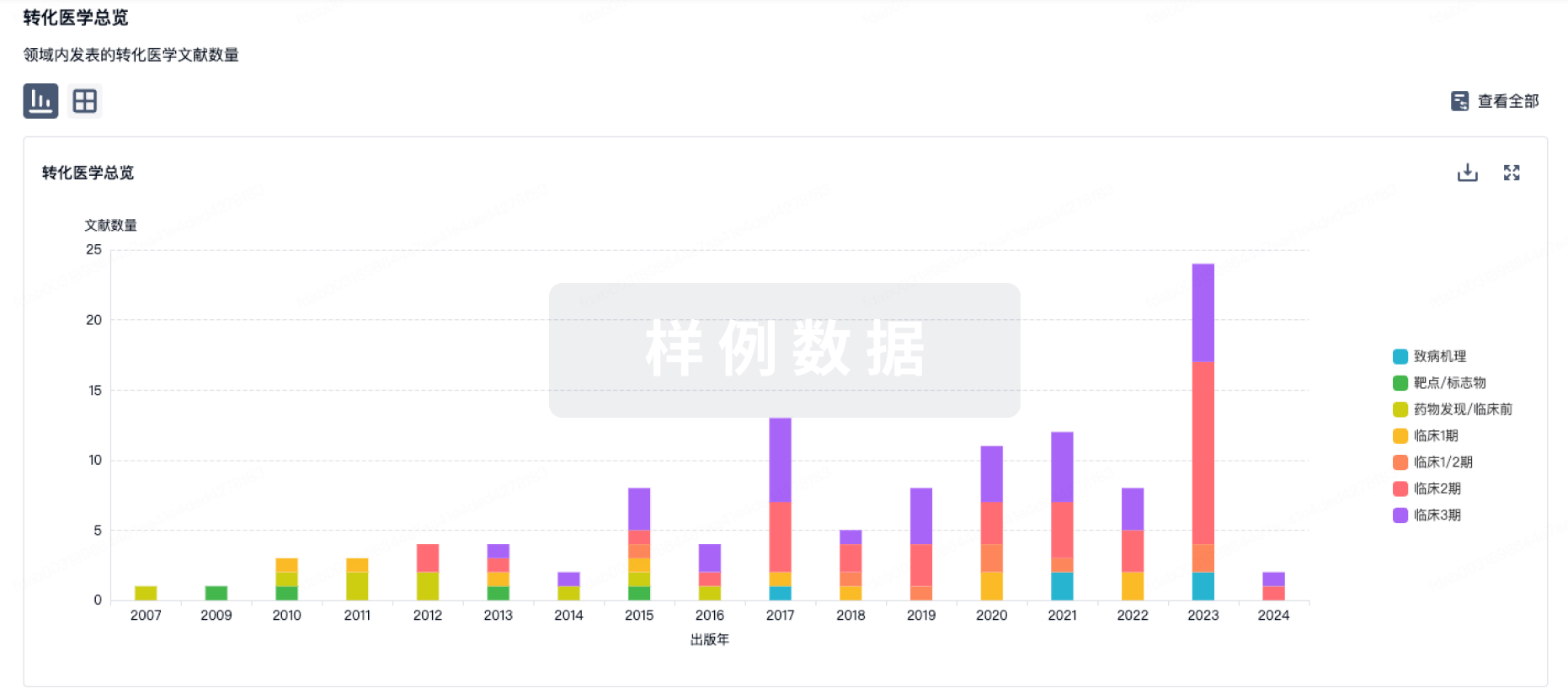
100 项与 CD7 CAR-T(Guangzhou Bio-gene Technology) 相关的转化医学
登录后查看更多信息
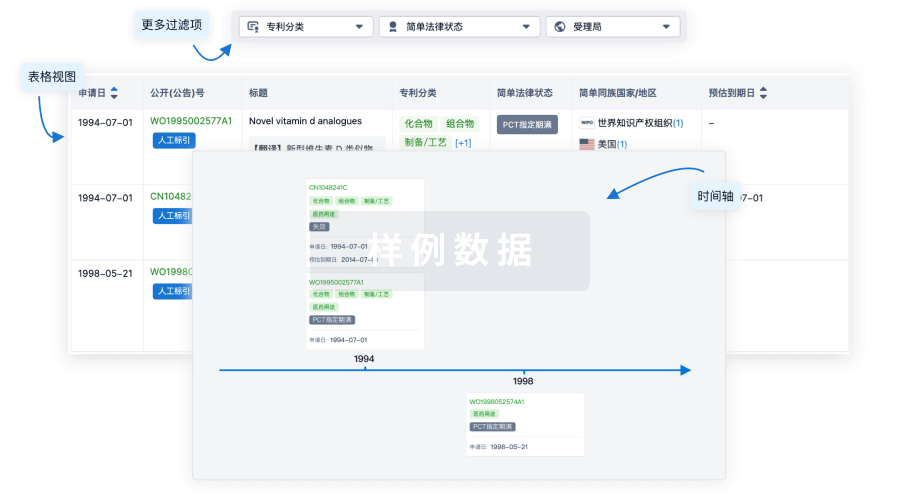
100 项与 CD7 CAR-T(Guangzhou Bio-gene Technology) 相关的专利(医药)
登录后查看更多信息
16
项与 CD7 CAR-T(Guangzhou Bio-gene Technology) 相关的文献(医药)2025-04-01·Clinical Lymphoma Myeloma & Leukemia
SOHO State of the Art Updates and Next Questions | CD7 CAR-T Therapy for Treating CD7-Positive Hematological Malignancies: Clinical Advances and Future Directions
Review
作者: Long, Jing ; Lu, Peihua
CD7 CAR-T cell therapy has emerged as a promising treatment for relapsed/refractory (R/R) CD7-positive hematological malignancies, offering new hope for patients with limited therapeutic options. This review examines the recent clinical advances, challenges, and future directions of CD7 CAR-T therapy. Clinical trials have demonstrated remarkable efficacy of CD7 chimeric antigen receptor T (CD7 CAR-T) cells in treating T-cell acute lymphoblastic leukemia (T-ALL), T-cell lymphoblastic lymphoma (T-LBL), and other CD7-positive malignancies, with complete remission (CR) rates of 90-95% in bone marrow (BM) and 50% to 60% in extramedullary disease (EMD). Various engineering strategies, including naturally selected CD7-targeted CAR-T cells, gene editing, protein blockers and universal CAR-T cells, have been developed to overcome challenges such as fratricide. While CD7 CAR-T therapy has shown promising initial responses, durable remissions often depend on consolidative allogeneic hematopoietic stem cell transplantation (allo-HSCT). Ongoing research is focused on optimizing CAR designs, improving CAR-T cell persistence, and developing novel combination strategies to enhance long-term outcomes. Safety profiles have been generally manageable, with cytokine release syndrome (CRS) and neurotoxicity being the primary concerns. However, prolonged cytopenias and potential long-term immunodeficiency due to depletion of healthy CD7-positive cells remain areas of active investigation. As CD7 CAR-T therapy continues to evolve, future directions include refining patient selection, exploring dual-targeting approaches, and investigating innovative strategies to integrate CAR-T therapy with allo-HSCT. These advancements aim to improve the efficacy, safety, and accessibility of CD7 CAR-T therapy for patients with CD7-positive hematological malignancies.
2025-03-06·BLOOD
CD7 CAR-T: a bridge to transplant in AML
Communications
作者: Mamonkin, Maksim
2025-02-01·Transplantation and Cellular Therapy
CD7 CART Therapy Bridging Allo-HSCT Remarkably Improves Long-Term DFS in Refractory/Relapsed T-ALL/LBL
Article
作者: Yang, Keyan ; Wang, Jingjing ; Wen, Wiaopei ; Li, Zhihui ; Chen, Chen ; Xu, Teng ; Wang, Xianxuan ; Zhao, Yongqiang ; Wu, Tong ; Zhou, Qi ; Zheng, Qinlong ; Song, Yanzhi ; Wang, Lei
T-ALL is caused by abnormal proliferation of T cells. It comprises 25%-50% of ALL cases in children and adults. Outlook for R/R T-ALL/LBL and patients over 60 is even dimmer. The treatment is challenging due to its biological and genetic diversity, limiting the development of effective targeted and immunotherapeutic strategies. Salvaged allo-HSCT offers only 20% to 30% DFS. This current study retrospectively analyzed 90 patients with R/R T-ALL (40, 44.4%) or T-LBL (50, 55.6%) treated at Beijing Gobroad Boren Hospital from February 2018 to January 2023. The median age was 14 (range: 2-65) y old. Somatic and germline gene mutations were detected by sequencing pretransplant. Thirty-two (35.6%) patients were sensitive to chemotherapy and achieved CR before transplant (CR group), and 58 (64.4%) cases were resistant to chemotherapy and in non-remission (NR) pre-HSCT. Forty-one of 58 patients in NR received CD7 CAR-T before allo-HSCT (CART group) and the rest 17 patients in NR underwent salvaged transplant (NR group). The results indicate that CD7 CAR-T group have OS (p = .029; 2-y OS rates: 54.4% [95% CI: 38.9% to 76%]) and DFS (p = .00032; 2-y DFS: 51.0% (95% CI: 36.9% to 70.7%)) similar to those in the CR group, but better than those in the NR group. The CIR for CD7 CAR-T group and CR group was significantly lower than NR group after 1 y (p = .0016; CAR-T group 2-y CIR: 31.67% (95% CI: 19.3% to 49.2%)). Our study examined the somatic and germline gene mutations in R/R T-ALL/LBL and evaluated the prognosis after transplantation. Based on our limited study, we found that using CD7 CAR T cells followed by allo-HSCT greatly enhanced the long-term DFS of chemo resistant T-ALL/LBL patients.
11
项与 CD7 CAR-T(Guangzhou Bio-gene Technology) 相关的新闻(医药)2025-03-31
EBMT 20253月30日,意大利佛罗伦萨——这座文艺复兴的摇篮,迎来了第51届欧洲血液与骨髓移植学会年会(EBMT 2025)的盛大开幕。作为全球血液学领域极具影响力的国际盛会,本届大会吸引全球超5000位专家学者共襄盛举,共探造血干细胞移植与细胞治疗的前沿进展。在大会首日,《肿瘤瞭望-血液时讯》十分荣幸邀请到哈尔滨血液病肿瘤研究所所长马军教授,介绍本届大会的精彩亮点、中国专家的卓越成果以及AI技术带来的颠覆性变革,并高屋建瓴地指出中国血液移植领域的未来方向。大会精彩亮点三大先进药物成为主战场《肿瘤瞭望-血液时讯》马教授,您好!今年再次来到EBMT大会现场有哪些不同的感受?本次会议上有哪些亮点尤为值得国内同道关注?马军教授今年是疫情后我们第四次参加欧洲血液与骨髓移植学会(EBMT)年会,也是规模最大的一次。根据相关资料和EBMT大会主席介绍,今年参会人数超过5800人。中国代表团的参会人数较前年增长了一到两倍,注册人数接近100人,实际到会80余人。中国学者的口头报告和壁报展示占大会总量的20%左右。EBMT大会主席特别提到,中国已融入国际大家庭,尤其在CAR-T细胞治疗方面作出了突出贡献,与欧美国家并肩齐驱,在国际舞台上占据重要位置。此次会议的核心议题之一就是CAR-T细胞治疗的快速进展。目前,我们提倡的先进药物包括三种:(1)细胞治疗:包括自体CAR-T、异体CAR-T、通用型CAR-T,以及肿瘤浸润淋巴细胞(TIL)和自然杀伤细胞(NK)等免疫细胞疗法。(2)基因治疗:从早期的病毒载体(RV)技术到转基因技术,再到如今备受关注的mRNA技术,基因治疗已逐渐在血液系统疾病、肿瘤和罕见病治疗中占据重要地位。(3)干细胞治疗:尽管全球已完成4000多项干细胞相关临床试验,但真正进入临床应用的仍属少数。干细胞并非万能,其在罕见病治疗、造血干细胞移植等领域已较为成熟,但在其他领域的应用仍需更多研究支持。本次会议仍以造血干细胞移植为主,同时涉及关节修复、心脏疾病、神经系统疾病以及抗衰老等领域的干细胞应用。过去,EBMT大会主要聚焦于造血干细胞移植(包括全相合、半相合、自体移植及脐带血移植),而近年来,细胞治疗和基因治疗已逐步成为会议的核心议题,共同构成了CGT(即细胞治疗、基因治疗、干细胞治疗)的主战场。今年,细胞治疗相关议题占比超过20%。在黄晓军院士“北京方案”的引领下,造血干细胞移植技术已发展到“人人都有供者”的时代。全球每年进行超过10万例移植手术,为白血病、淋巴瘤和其他血液系统肿瘤患者提供了治愈希望。在细胞与基因治疗领域,美国已批准13个CAR-T产品和近40个CGT相关药物,而中国目前批准了6个CAR-T产品。中国正加速推进先进药物的研发与审批,相关评审制度和指导原则预计今年出台。此次会议的参会者较往年增加了30%以上,主要就是聚焦在细胞治疗和基因治疗方面。造血干细胞移植已走向细胞治疗和基因治疗的新前沿,本次会议聚焦细胞治疗、基因治疗和干细胞治疗议题,吸引了众多临床医生、基础研究者、生物制药企业高管以及转化医学领域的专家。总之,中国已融入世界,加强国际交流与合作,不仅是推动中国医学进步的必要途径,更是为全球血液肿瘤和罕见病患者贡献力量的重要方式。我们始终秉持“生命至上”的原则,以患者为中心,努力实现更高的临床治愈率和生存质量。期待此次会议带来更多突破性成果,为全球患者带来新的希望。与国际融合中国血液学的高光时刻《肿瘤瞭望-血液时讯》本次大会上,中国专家团队的研究成果从量到质都令人瞩目。那么,其中哪些研究给您留下了深刻印象,您如何看待中国在全球血液移植领域的地位和贡献?马军教授今年中国专家的报告占据大会整体报告的20%左右。中国在细胞治疗领域的进展令人瞩目,特别是在CAR-T、CAR-NK、通用型和自体型细胞治疗技术方面的进展十分迅速。中国对髓系白血病的治疗研究取得了重要突破,CD7 CAR-T治疗复发/难治性T细胞淋巴瘤已进入临床研究阶段。此外,中国已批准6个CAR-T产品,数量超过欧洲,覆盖了急性淋巴细胞白血病、淋巴瘤、多发性骨髓瘤等多种疾病领域。最近,中国还与美国同步批准了一项间充质干细胞治疗急性移植物抗宿主病(GVHD)的临床研究。在基因治疗领域,中国预计很快将有首个基因治疗产品获批上市。EBMT主席在与我交流时表示,中国在细胞治疗和半相合移植方面作出了突出贡献,期待中国未来能为全球医学发展提供更多新技术和解决方案。此次会议吸引了包括黄晓军院士、吴德沛教授、刘启发教授、黄河教授和姜尔烈教授等在内的多位中国顶级移植和细胞治疗领域专家。大家此行的主要目的是通过与国际同行的深入交流与接轨,为中国患者在细胞治疗和干细胞移植领域作出更多贡献,让中国患者真正获益。学术交流是推动医学进步的重要动力。正如我们常说的“学术无止境,科学无国界”,只有通过开放的学术交流,才能为血液淋巴系统肿瘤的未来带来更多的可能性。我们期待明天中国代表团的报告为大会带来更多亮点,为全球学术界贡献更多的中国智慧和力量。AI赋能血液学从诊断到治疗的智能化变革《肿瘤瞭望-血液时讯》今年年初,国产AI大模型DeepSeek火爆全球,在本次会议上,也有多个关于AI的专题,您认为AI将对血液移植领域带来哪些变革?马军教授AI技术近年来发展迅猛,尽管它尚未达到完全替代人类医生的能力,尤其在与顶级专家和经验丰富的医生相比仍存在局限性,但其潜力不可忽视。中国在AI技术创新方面表现突出,我们正努力借助AI技术、计算机技术、机器人设备以及大数据来更深入地了解患者,这在现代医疗中至关重要。循证医学的目标是为未来的治疗奠定基础,而AI技术则通过大数据的集中化、精细化和亚专科化,为特殊病和常见病的治疗提供了新的可能性。在本次会议上有四个AI技术相关高峰论坛,我们将通过这些论坛着重了解国际上尤其是欧洲和美国如何将AI技术应用于血液淋巴瘤领域。在形态学和病理学中,AI技术已被广泛采用。以恶性淋巴瘤为例,该疾病有148个亚型,传统的人类分析需要四年才能完成一次数据更新,而通过AI技术,这一周期已缩短至三个月。此外,AI技术在特殊亚型的病理结构分析、免疫组化、二代测序以及基因突变检测方面也展现出了惊人的效率,为临床提供了快速而精准的结果。因此,我认为对于淋巴瘤而言,AI技术将在病理分类、基因分型以及微小残留病(MRD)监测等方面发挥重要作用。在白血病领域,MRD技术被广泛用于评估患者的治愈可能性以及预测复发时间。通过大数据分析,我们可以更清晰地了解不同亚型的复发规律和治疗效果,这为临床决策提供了重要参考。然而,我们不能完全依赖AI技术,而是需要将人类医生的智慧与AI技术相结合,只有这种人机协作才能推动科学进步,为肿瘤治愈带来希望。我们期待将AI技术深度融合到血液淋巴系统肿瘤的诊疗中。目前,这一领域的研究正在全球范围内积极推进。AI技术与医生的协作不仅能提升疾病的诊断、鉴别和治疗效果,还能在预后评估中发挥重要作用。这是一门新兴的学科,我们需要在多方面结合和考虑,既要充分利用AI技术的优势,也要避免过度依赖。只有这样,AI技术才能在血液淋巴系统肿瘤领域发挥最大效用,为患者、医生乃至全人类的健康福祉做出贡献。创新引领未来突破专利瓶颈与构建协作生态《肿瘤瞭望-血液时讯》最后,在与国际专家或团体的交流中,您认为我国在造血干细胞移植或CAR-T治疗领域还存在哪些不足?未来需要从哪些方面进一步努力?马军教授中国在血液系统疾病和造血干细胞移植领域取得了显著成就,例如黄晓军院士的半相合移植技术,已获得国际专利认可;亚砷酸和全反式维甲酸技术也处于世界领先地位。然而,在细胞治疗领域,中国的专利数量相对较少,美国已有近千项相关专利,中国在这一领域的创新仍显不足,大多数研究仍停留在Me-better阶段,而First-in-Class的创新则非常少。我希望能够发展中国自己的细胞治疗技术和CGT技术。在成立中国临床肿瘤学会(CSCO)时,我们确立了“团结协作、务实创新”的宗旨,这八个字相辅相成,缺一不可。然而,目前我们在原始创新方面仍有较大差距,虽然能够快速跟进国际前沿,实现弯道超车,但必须脚踏实地、一步一个脚印地推进。我希望年轻科学家、医生以及转化医学、基础医学、生物学领域的专家能够携手合作,组建跨学科大团队,以患者为中心、以创新为驱动,共同努力推动中国细胞治疗技术的发展,让中国在这一领域在全球占据一席之地。尽管今年我们的报告占到了大会的20%,细胞治疗相关议题占到了50%,但我们仍需清醒地认识到,与发达国家和顶尖生物研究机构相比,我们仍存在明显差距。中国最大的短板在于协作、团结和转化精神的缺乏,这导致我们在Cell、Nature等顶级期刊上发表的高质量研究,往往难以转化为临床应用。我曾统计过诺贝尔奖的获奖情况,发现17位临床医生的获奖成果无一例外都是基于创新药物或创新治疗方法,例如mRNA技术、艾滋病鸡尾酒疗法、DNA技术和造血干细胞移植技术。这充分说明,临床医生是转化医学的主力军,是推动医学进步的一线战士。只有通过协作、交流、团结和创新,我们才能让中国的细胞治疗和造血干细胞移植技术达到世界先进水平,为全球患者贡献中国智慧和力量。我们希望老中青血液学学者能够联合起来,团结务实、协作创新,为中国医学的未来而努力。会场花絮专家简介马军 教授哈尔滨血液病肿瘤研究所所长主任医师,教授,博士生导师哈尔滨血液病肿瘤研究所所长中国临床肿瘤学会(CSCO)监事会监事长亚洲临床肿瘤学会副主任委员中国临床肿瘤学会白血病专家委员会主任委员国家卫生健康委能力建设与继续教育中心淋巴瘤专科建设项目专家组组长白血病·淋巴瘤杂志 总编辑原中国临床肿瘤学会(CSCO)主任委员原中华医学会血液学分会副主任委员(来源:《肿瘤瞭望–血液时讯》编辑部)声 明凡署名原创的文章版权属《肿瘤瞭望》所有,欢迎分享、转载。本文仅供医疗卫生专业人士了解最新医药资讯参考使用,不代表本平台观点。该等信息不能以任何方式取代专业的医疗指导,也不应被视为诊疗建议,如果该信息被用于资讯以外的目的,本站及作者不承担相关责任。
细胞疗法基因疗法免疫疗法信使RNA临床研究
2025-01-14
·美通社
北京
2025年1月14日
/美通社/ -- 近日,陆道培医院陆佩华院长作为第一作者和通讯作者,在国际血液学权威期刊Blood(IF=21)在线发表了题为"Nanobody-based Naturally Selected CD7-Targeted Chimeric Antigen Receptor T Cell Therapy for Acute Myeloid Leukemia"的研究论文。这项研究成果标志着在急性髓系白血病(AML)治疗领域的又一重大突破。
在该研究中,陆佩华院长带领团队创新性地采用基于纳米抗体的CD7 CAR-T治疗急性髓系白血病,研究结果不仅在肿瘤杀伤力和安全性上取得了显著进展,更为难治复发急性髓系白血病的治疗开辟了新路径。
研究背景
难治或复发(R/R)急性髓系白血病(AML)预后相对较差,即使接受异基因造血干细胞移植(allo-HSCT)的患者中也是如此,迫切需要的新的疗法。大约30%的AML患者在恶性肿瘤细胞上表达CD7。我们中心之前已经发表了相关文章,证明了自然选择的CD7 CAR-T(NS7CAR-T)疗法在T细胞淋巴恶性白血病中表现出显著疗效,且安全性良好。
嵌合抗原受体(CAR)的传统靶向域依赖于单克隆抗体(mAbs)中的IgG变量区域的单链片段(scFv)。最近,一种利用羊驼科重链抗体的单变量域,即所谓的纳米抗体,作为一种替代方法,已经变得越来越重要。纳米抗体的分子大小(15kDa)大约是人IgG分子的十分之一。虽然传统的mAbs需要六个互补决定区(CDRs)来结合抗原,但纳米抗体仅用三个CDRs就能维持相当的亲和力和特异性。此外,由于它们与人类VH基因家族III的相似性,纳米抗体比小鼠mAbs表现出更低的免疫原性。值得注意的是,一个成熟的表面展示平台也促进了能够针对同一抗原的不同表位的多个纳米抗体的生成,传统mAbs在这方面通常表现出比较有限的能力。而且,特别相关的是,基于纳米抗体的CAR-T显示出增强的效应细胞因子释放。我们采用了纳米抗体技术来生产NS7CAR-T细胞。在此文章中,我们报告了Nanobody-based NS7CAR-T产品的临床前研究数据,以及在一项I期临床试验中(
https://clinicaltrials.gov
NCT04938115) Nanobody-based NS7CAR-T治疗难治/复发CD7阳性急性髓系白血病(AML)中的安全性和有效性结果。
研究方法
基于纳米抗体的dVHH NS7CAR包含两个抗CD7纳米抗体(VHHs)的编码区域,这些区域通过一个连接子(G4S)
5
连接在一起,以及CD8α铰链区域、CD8α跨膜域,还有一个第二代CAR细胞骨架,其在细胞内共刺激域包含4-1BB和CD3ζ。制备时,通过白细胞采集术获得外周血(PB)单核细胞,分离T细胞并用慢病毒转导。第二代CD7CAR由抗CD7单链抗体、IgG4铰链区、CD28TM跨膜结构域、4-1BB和CD3ζ的胞内共刺激结构域及截短EGFR蛋白通过T2A连接构成。所有患者在CD7CAR-T回输3天前静注氟达拉滨(30 mg/m
2
/d)和环磷酰胺(300 mg/m
2
/d)。从采集到CAR-T细胞输注的中位时间为15天。
研究结果
首先是临床前研究,dVHH NS7CAR-T和传统scFV NS7CAR的
结构对比
。研究发现,dVHH NS7CAR-T细胞在培养大约两周后显示出比scFv NS7CAR-T更强的扩增能力(23.9 folds vs.8.1 folds,P=0.024)。
在不同的效应细胞与靶细胞比例下,scFv和dVHH NS7CAR-T细胞对KG1a靶细胞表现出相似的抗恶性细胞的功能。流式细胞术(FCM)、逆转录聚合酶链反应(RT-PCR)和蛋白印迹(WB)分析表明,scFv NS7CAR-T和dVHH NS7CAR-T细胞都没有在它们的细胞表面检测到流式细胞术可检测的CD7表达,然而通过RT-PCR和WB检测到了显著的CD7 mRNA和蛋白水平。dVHH NS7CAR-T细胞显示出强大的抗肿瘤活性,在输注后第8天表现出显著的抗肿瘤活性。而接受PBS或对照T细胞治疗的小鼠肿瘤生长迅速。
在此I期临床试验中,共入组了12例CD7阳性R/R AML(CD7表达率>50%,强度良好),最后10例患者接受了dVHH NS7CAR-T细胞输注,其中4例输注了5×10
5
/kg,6例输注了1×10
6
/kg。中位年龄为34岁(7-63岁),入组时骨髓的肿瘤负荷中位值为17.0%(2.0-72.7%)。1例患者同时有髓外病变(EMD)。入组前,患者曾经接受的治疗中位线数为8(3-17)。而且,7例患者有造血干细胞移植史,从上次移植到复发的中位间隔期为12.5个月(3.5-19.5个月)。
在dVHH NS7CAR-T细胞输注后28天评估,7/10(70%)患者在骨髓中实现了完全缓解(CR),其中6人达到了微小残留病灶(MRD)阴性CR。3例患者无效(NR),其中1例EMD患者根据第35天的PET-CT评估达到部分缓解(PR)。所有NR患者发现CD7抗原丢失。中位随访时间为为178天(28-776天)。对于7例CR患者,3例在CD7 CAR-T细胞输注约2个月后接受了巩固性第二次异基因造血干细胞移植。一例患者在随访401天仍处于缓解状态,而其他2例患者分别于241天和776天死于非复发原因、肾衰及感染。对于其他4例没有桥接移植的患者,3例分别于第47天、第83天和第89天复发(3例患者复发时CD7均丢失),另外1例患者死于肺部感染。
关于安全性,大多数患者(80%)出现轻度细胞因子释放综合征(CRS),7例患者呈I级,1例呈II级CRS,而2例患者(20%)呈III级CRS。没有神经毒性的发生。在7例有移植史的患者中,1例(为在之前移植后约100天后复发的患者)在CAR-T治疗后出现轻度皮肤移植物抗宿主疾病。
结论
我们的研究说明dVHH NS7CAR-T疗法可以使难治复发的AML患者再次达到初步的完全缓解,即使是对于之前接受过多线治疗以及移植后复发的AML患者,NS7CAR-T治疗的安全性是可控的。在dVHH NS7CAR-T疗法后,巩固性异基因造血干细胞移植(allo-HSCT)在我们的试验中仍然在维持长期疗效方面发挥作用。
CD7抗原丢失是不缓解或复发患者的一个主要问题,我们发现5/6例伴有double CEBPA突变的AML患者在后续丢失了CD7抗原,显示出较差的预后,这提示在以后CD7CAR-T治疗AML的临床试验中可能要考虑是否排除这类患者。
最后,为了更好评估纳米抗体基础的NS7CAR-T在治疗CD7阳性AML方面的疗效和安全性,需要纳入更多的患者和随访更长时间来进一步证实。
急性髓系白血病(AML)是一种复杂且异质性极高的血液恶性肿瘤,现有治疗方案的局限性使其长期缓解率和总体生存率仍面临严峻挑战。陆佩华院长带领团队创新性通过基于纳米抗体的自然选择CD7靶向嵌合抗原受体T细胞疗法在急性髓系白血病的治疗中,展现了优异的治疗效果和较低的脱靶毒性,其详尽的数据支持得到了国际同行的高度评价。
这一成果的发表,不仅为急性髓系白血病患者带来了新的希望,也再次展示了陆道培医学团队在全球血液学研究领域显著的学术地位。未来,陆道培医学团队将继续深耕血液病的基础与临床研究,不断推动科学成果的转化应用,为全球血液病患者带来更多福音。
临床1期细胞疗法免疫疗法临床终止
2025-01-13
T细胞急性淋巴细胞白血病和外周T细胞淋巴瘤是常见的T细胞血液肿瘤,复发/难治性T细胞恶性肿瘤具有高异质性和不良预后。CAR-T细胞疗法在治疗B细胞源性恶性肿瘤中显示出显著的安全性和有效性,但在治疗T细胞恶性肿瘤有局限性较大,如自相残杀、T细胞发育不全、肿瘤污染等,主要是因为正常T细胞与恶性T细胞的相似性而缺乏明确的恶性T抗原。CAR靶向抗原可分为泛T抗原和限制性T抗原,两者各有优缺点;泛T抗原CAR-T细胞(如CD5和CD7靶点)是临床试验中应用最广泛的CAR-T细胞,几乎可以覆盖所有T细胞来源的恶性细胞,但也可以诱导CAR-T细胞和正常T细胞的严重杀伤。与自体来源的CAR-T细胞相比,异体CAR-T细胞可以防止肿瘤污染,并通过基因编辑成为通用产品,然而这些CAR-T细胞都不能完全预防靶向T细胞CAR-T细胞治疗后的免疫缺陷和疾病复发。
浙江大学医学院附属第一医院学者近日于《Experimental Hematology & Oncology》综述,总结了目前CAR-T细胞治疗T细胞恶性肿瘤的挑战以及解决这些局限性的潜在策略,通讯作者为黄河教授和胡永仙教授。现整理主要内容供参考。
CAR-T细胞治疗T细胞恶性肿瘤的当前挑战
针对T细胞源性恶性肿瘤的理想CAR-T细胞靶抗原应在所有恶性T细胞表面高度表达,但在正常组织上不表达。然而T细胞恶性肿瘤通常异质性较强,所有肿瘤细胞中都存在最佳抗原的情况极为罕见。此外,如果CAR-T细胞与正常T细胞具有相同的抗原,就会识别并消灭所有三种类型的细胞:恶性T细胞、其他CAR-T细胞和正常T细胞。
CAR-T细胞之间的杀伤也被称为自相残杀,可能导致CAR-T细胞在体内扩增、持续和抗肿瘤效果差。CAR-T细胞输注引起的T细胞发育不全目前尚无有效的治疗方法,并可能增加患者生命危险的机会性感染。由于恶性T细胞通常存在于T-ALL患者和部分T细胞淋巴瘤(TCL)患者的外周血中,并且与正常T细胞具有相同的表面抗原,因此完全有可能收集恶性T细胞进行CAR转导。因此CAR-T细胞可能被恶性T细胞污染,导致CAR-T细胞治疗过程中的抗原逃逸。
T细胞恶性肿瘤的潜在靶抗原
T细胞恶性肿瘤的靶抗原可分为覆盖所有T细胞的抗原和局限于T细胞亚群的抗原。
泛T抗原CAR-T细胞(如CD5和CD7靶点)是临床试验中应用最广泛的CAR-T细胞,几乎可以覆盖所有T细胞来源的恶性细胞,但也可以诱导CAR-T细胞和正常T细胞的严重杀伤。CAR-T细胞的自相残杀作用和on-target off-tumor作用可导致CAR-T细胞在治疗过程中持续时间有限和重度T细胞发育不全,最终影响CAR-T细胞的疗效。有多种新兴技术可以避免自相残杀和T细胞发育不全,例如基因编辑、蛋白保留、瞬时CAR表达技术和安全开关,但需要全面的临床试验来评估每种技术的可行性和安全性。
局限于特定T细胞亚群的抗原(例如CD4、TRBC1、TRBC2、CD1a、CD30、CD37、CD21、CCR4和CCR9,正处于临床前和临床研究阶段)可以部分避免严重的自相残杀和T细胞发育不全,但目前关于限制性抗原CAR-T细胞的研究很少,此外必须谨慎筛选合适的肿瘤类型。此外,对每例打算接受CAR-T细胞治疗的患者进行抗原筛查有助于识别最佳抗原。
自体和异基因CAR-T用于T细胞肿瘤
CAR-T细胞的另一种分类包括自体和异基因CAR-T细胞。自体T细胞没有GvHD或排斥反应,但肿瘤污染是主要问题。相比之下,异基因CAR-T细胞具有高纯度、高质量和无肿瘤污染,但异基因过继输注存在局限性包括GvHD和异基因排斥反应。一般来说,异基因CAR-T细胞可以分为四种类型:HSCT供者细胞(来自以前的HSCT供者的细胞)、人类白细胞抗原(HLA)全相合供者细胞(来自HLA全相合供者的细胞)、单倍体相合供者细胞(来自单倍相合供者的细胞)和通用细胞(来自非亲缘、健康供者的细胞)。鉴于无GvHD和毒性较小,自体CAR-T细胞可能更推荐用于低肿瘤负荷患者。需要更多的临床研究来分析自体和异异基因CAR-T细胞的优缺点,以帮助临床医生在未来不同的临床情况下进行选择。
尽管基因编辑的通用CAR-T细胞可以解决肿瘤污染、GvHD和异基因移植排斥等问题,但与CRISPR/Cas9系统相关的遗传毒性风险也不应被忽视。碱基编辑是一种更安全的编辑工具,因为它不依赖于双链DNA断裂,可以成为逃避遗传毒性的理想基因编辑手段。对于通用CAR-T细胞来说,体内持久性仍存在挑战。通用CD7 CAR-T细胞治疗后恢复的CD7阴性T细胞可以抵抗CAR-T细胞的杀伤,并在CAR-T细胞的异异基因排斥中发挥作用,可能是通用CD7 CAR-T细胞在体内存活时间短的原因。期望将来有更多的方法来延长通用CAR-T细胞在T细胞来源的恶性肿瘤中的体内持久性,以获得更好的临床结局。
CAR-T治疗T细胞肿瘤的并发症
CAR-T治疗T细胞肿瘤后的主要并发症包括CRS、ICANS、移植物抗宿主病、插入突变、第二肿瘤,部分并发症是靶向T 细胞CAR-T细胞治疗所特有的,如T细胞发育不全(aplasia)引起的机会性感染(如EBV和CMV再激活)、骨髓抑制引起的持续性血细胞减少、靶抗原阴性复发(如CD7阴性复发)。
T细胞发育不全是治疗T细胞源性恶性肿瘤的主要挑战,可导致不受控制的机会性感染并威胁到患者生命。CD7阴性T细胞的起源和功能尚不清楚,应进一步探索CD7缺失的T细胞(特别是CD7 CAR-T细胞治疗后新出现的CD7阴性T细胞)是否仍然对机会性感染具有抵抗力,或者如何提高这类T细胞的功能,以提高患者生存。
治疗抗原阴性复发的策略包括改变CAR-T抗原、双靶点CAR-T、桥接移植巩固;桥接移植方面,作者团队开发了一种新的策略,将CD7 CAR-T治疗序贯单倍体HSCT,不进行GvHD预防,为不适合异基因移植的CD7阳性恶性肿瘤患者提供了一种替代方法。整体而言,还没有有效的策略来预防或治疗疾病复发,特别是抗原阴性复发,对靶向T细胞CAR-T治疗后复发机制的深入探索可能有助于解决该问题。
参考文献
Zheng, H., Zhao, H., Han, S. et al. Chimeric antigen receptor-T cell therapy for T cell-derived hematological malignancies. Exp Hematol Oncol 13, 117 (2024). https://doi-org.libproxy1.nus.edu.sg/10.1186/s40164-024-00584-6
识别微信二维码,添加生物制品圈小编,符合条件者即可加入
生物制品微信群!
请注明:姓名+研究方向!
版
权
声
明
本公众号所有转载文章系出于传递更多信息之目的,且明确注明来源和作者,不希望被转载的媒体或个人可与我们联系(cbplib@163.com),我们将立即进行删除处理。所有文章仅代表作者观点,不代表本站立场。
细胞疗法免疫疗法
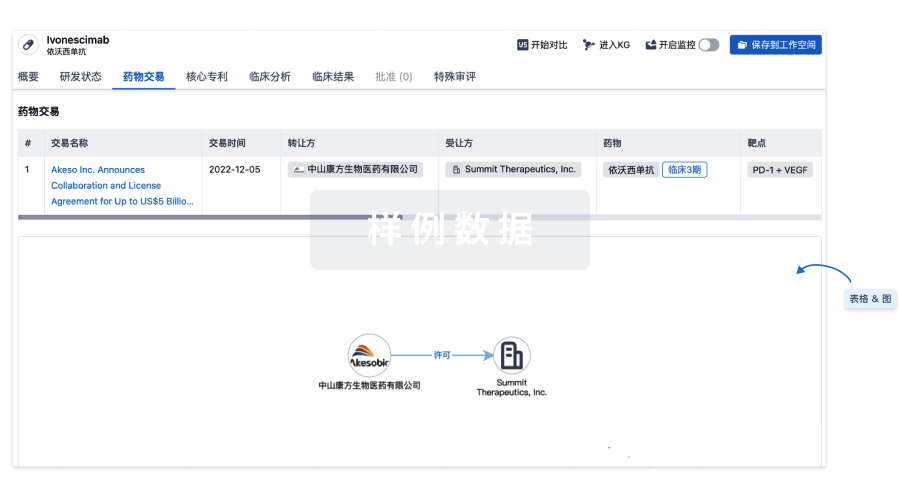
100 项与 CD7 CAR-T(Guangzhou Bio-gene Technology) 相关的药物交易
登录后查看更多信息
研发状态
10 条进展最快的记录, 后查看更多信息
登录
| 适应症 | 最高研发状态 | 国家/地区 | 公司 | 日期 |
|---|---|---|---|---|
| 难治性 T 急性淋巴细胞白血病 | 临床2期 | 中国 | 2023-05-01 | |
| T细胞急性淋巴细胞白血病/淋巴瘤 | 临床2期 | 中国 | 2023-05-01 |
登录后查看更多信息
临床结果
临床结果
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
核心专利
使用我们的核心专利数据促进您的研究。
登录
或
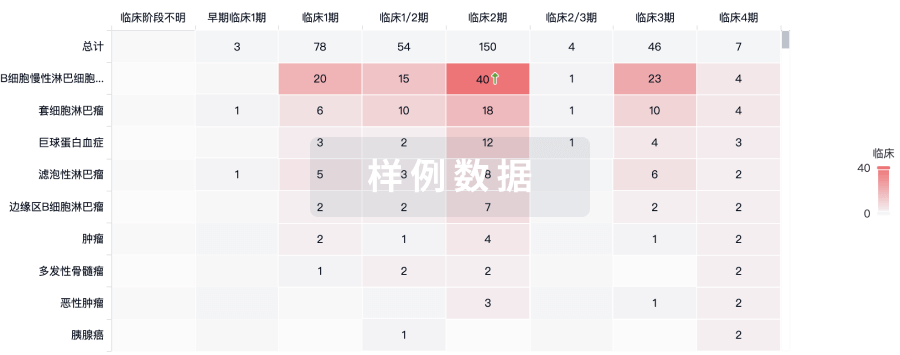
临床分析
紧跟全球注册中心的最新临床试验。
登录
或
批准
利用最新的监管批准信息加速您的研究。
登录
或

特殊审评
只需点击几下即可了解关键药物信息。
登录
或

Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用
