预约演示
更新于:2025-10-12
Tolnaftate
托萘酯
更新于:2025-10-12
概要
基本信息
非在研机构- |
权益机构- |
最高研发阶段批准上市 |
最高研发阶段(中国)- |
特殊审评- |
登录后查看时间轴
结构/序列
分子式C19H17NOS |
InChIKeyFUSNMLFNXJSCDI-UHFFFAOYSA-N |
CAS号2398-96-1 |
关联
100 项与 托萘酯 相关的临床结果
登录后查看更多信息
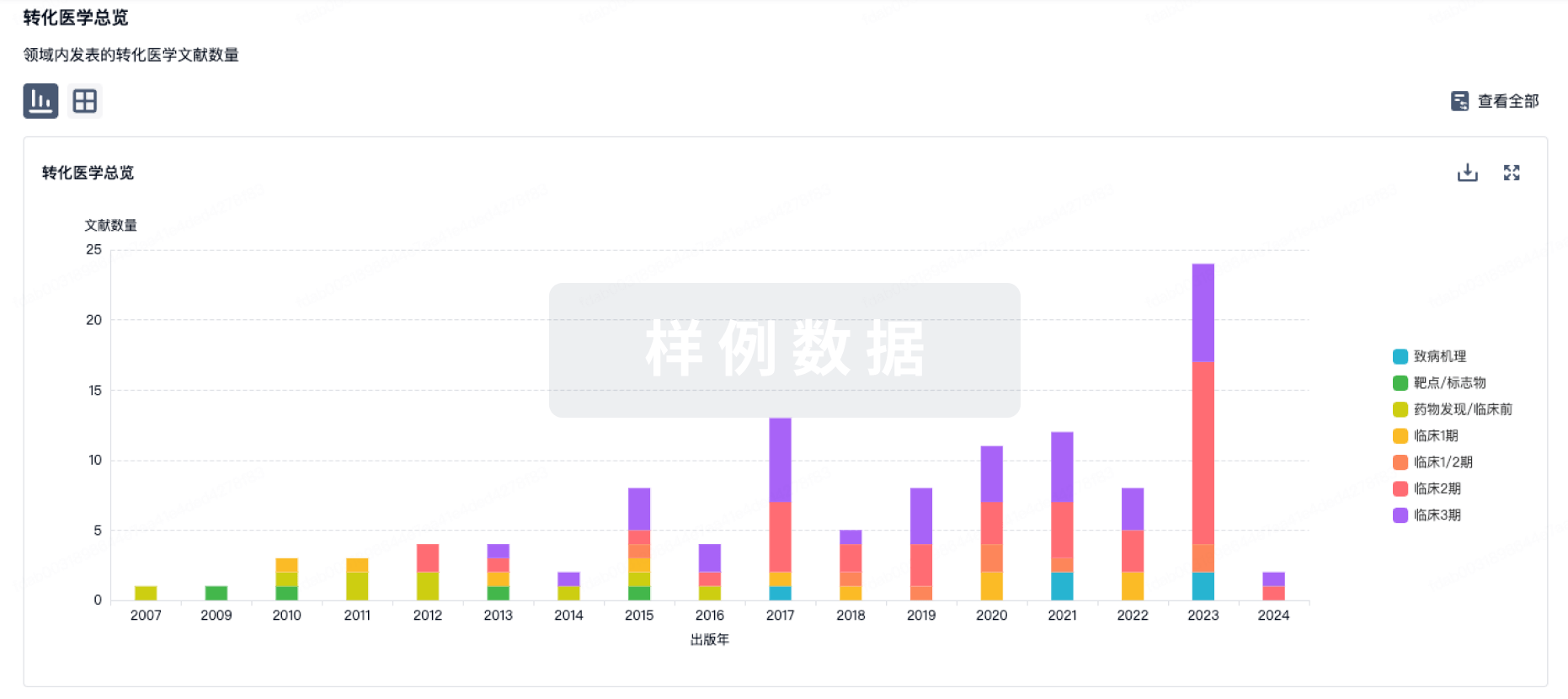
100 项与 托萘酯 相关的转化医学
登录后查看更多信息
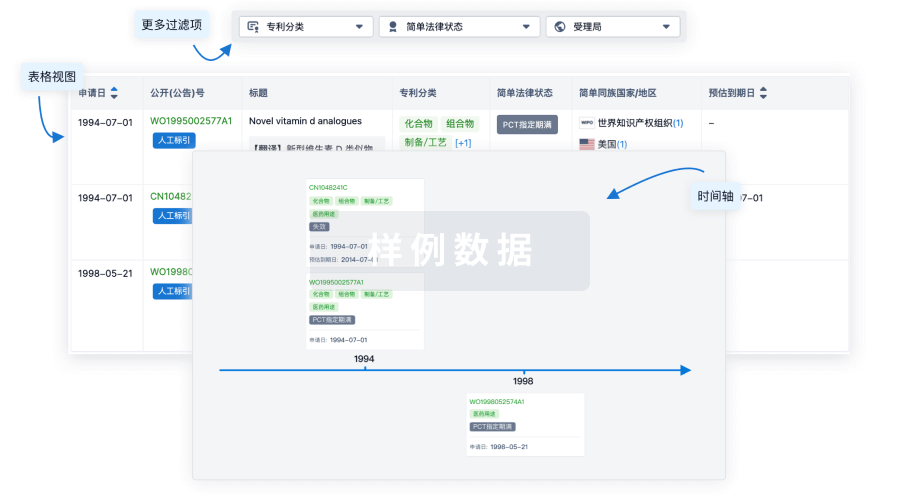
100 项与 托萘酯 相关的专利(医药)
登录后查看更多信息
376
项与 托萘酯 相关的文献(医药)2025-09-01·Cureus Journal of Medical Science
Innovation in Onychomycosis Treatment Through Creative Compounding.
Article
作者: Frey, Christian P ; Gorski, Matthew ; Hoffman, Kristine
Onychomycosis is a common fungal nail infection, often presenting with nail discoloration, thickening, and brittleness. Despite the availability of oral and topical antifungal agents, recurrence rates remain high, and systemic therapies can pose risks such as hepatotoxicity and drug interactions. This case report describes an innovative treatment approach using a compounded topical preparation made by combining a crushed 250 mg oral terbinafine tablet with an over-the-counter 1% tolnaftate nail lacquer. A healthy 28-year-old female presented with diffuse toenail onychomycosis affecting all digits. After declining oral therapy, she initiated daily application of the compounded lacquer for 10 months. Weekly complete removal and reapplication were performed, and the vial was shaken before each use to maintain a homogenous mixture. The patient documented progress photographically and reported high satisfaction with a significant improvement in nail appearance. No adverse effects were noted. This topical use of pulverized terbinafine takes advantage of the drug's favorable molecular profile for nail penetration, offering targeted treatment with minimal systemic absorption. The estimated daily delivery of terbinafine per nail was approximately 0.4 mg, a potentially therapeutic dose when applied consistently over time. This case supports the potential of creative compounding in expanding safe and patient-friendly treatment options for onychomycosis, especially for individuals who are unable or unwilling to take oral antifungals. Further studies are needed to evaluate the efficacy, pharmacokinetics, and broader applicability of this approach.
2025-08-01·JOURNAL OF CHEMICAL THERMODYNAMICS
Comments on “solubility determination, correlation, solvent effect and thermodynamic properties of tolnaftate in ten mono-solvents and binary solvent systems from 283.15 K to 328.15 K"
作者: Kabin, Allison ; Kumarandurai, Dhishithaa ; Lin, Bradley ; Acree, William E.
A polemic is given regarding the solution models used by Wang and coworkers to correlate the solubility behavior of tolnaftate in ten organic mono-solvents and in binary acetic acid + ethylene glycol solvent mixturesFor several of the mixtures studied authors' calculated curve-fit parameters yielded mole fraction solubilities that exceeded unity.
2025-06-01·JOURNAL OF CHEMICAL THERMODYNAMICS
Solubility determination, correlation, solvent effect and thermodynamic properties of tolnaftate in ten mono-solvents and binary solvent systems from 283.15 K to 328.15 K
作者: Wang, Xianxiang ; Xu, Funeng ; Lin, Juchun ; Ren, Yuanmo ; Wang, Kejia ; Shu, Gang ; Tang, Huaqiao ; Zhang, Wei ; Li, Haohuan ; Ai, Xiaoyang ; Lin, Shiyu ; Fu, Hualin ; Li, Ting
Tolnaftate (TNF) is a local antifungal agent.The determination of its solubility can serve as a valuable reference for its crystallization and formulation design, an area that has not yet been comprehensively investigated.In this study, the static method was carried out to determine the solubility of TNF in 10 mono-solvents (methanol, ethanol, n-propanol, isopropanol, n-butanol, isobutanol, n-octanol, 1,2-propanediol, ethylene glycol, acetic acid) and the binary mixed solvents (acetic acid + ethylene glycol) at T = (283.15 to 328.15) K and P = 0.1 MPa.The experiment results showed that TNF dissolves best in acetic acid and worst in ethylene glycol among investigated mono-solvents.And the solubility in mixed solvents was observed to increase as the mole ratio of acetic acid augments.In all solvents, there is obviously increase in the solubility of TNF as temperature elevates.The Apelblat model, van't Hoff model, Jouyban model, GCM model, Sun model and Apelblat-Jouyban-Acree model were used to fit the solubility values.And the root mean square deviation (RMSD) between the calculated values and exptl. values are less than 0.025%, showing that the exptl. values are accurate and the models have good fitting effects.At the same time, X-ray powder diffraction (PXRD) tests confirmed that the absence of crystal transformation during the process of TNF dissolutionIn addition, according to the KAT-LSER model, the influence of solute-solvent interactions on the solubility of TNF exceeds that of solvent-solvent interactions.The thermodn. properties including entropy (ΔH0sol), enthalpy (ΔS0sol), Gibbs free energy (ΔG0sol), enthalpy contribution (%ξH) and entropy contribution (%ξS) were calculated, which proved that dissolution process of TNF is endothermic and entropy-driven, and enthalpy mainly affects Gibbs free energy.
1
项与 托萘酯 相关的新闻(医药)2025-09-03
Clinically Tested Innovation Offers Powerful, Mess-Free Treatment, Symptom Relief and Prevention.
BOSTON, Sept. 3, 2025 /PRNewswire/ -- Propedix, an innovator in anti-infective topical dermatology treatments, announces the launch of
Dryello™ (tolnaftate 1%), a breakthrough over-the-counter antifungal treatment for Athlete's Foot (tinea pedis). Dryello's unique formulation, delivery approach, and application offer an entirely new way to treat and prevent Athlete's Foot —with a proprietary dry stick format that goes on dry and stays dry. The Dryello formulation is the first of numerous anti-infective products to emerge from Propedix's Stick-based DryStik Technology PlatformSM.
Continue Reading
Propedix Launches Dryello™, the First-Ever Dry Stick Antifungal for Athlete's Foot
Unlike traditional antifungal creams, sprays, and powders, Dryello features a clean, no-mess stick that delivers tolnaftate 1%, a proven antifungal active ingredient, in a portable, dry, deodorant-stick-like format. This first-of-its-kind innovative topical administration system is the first commercial product emerging from Propedix DryStik Technology PlatformSM. A unique and proprietary set of formulations designed to effectively deliver anti-fungal agents through an easy to administer dry applicator glide-on stick. Dryello eliminates the mess of traditional, old-school treatments and allows for delivery of the active agent in a patient-compliant manner. In the company's recent clinical study, 90% of patients who used Dryello were cured of Athlete's Foot, and 89% also reported less sweaty feet.*
Dryello was designed by board-certified dermatologist Dr. Carl Schanbacher and the R&D team at Propedix after years of development. "Dryello is redefining how we treat Athlete's Foot," said Dr. Schanbacher, CMO of Propedix. "Most antifungals add moisture, which can undermine treatment. Dryello applies dry, stays dry, and delivers powerful dual-action relief—treatment and prevention – all in a convenient stick." The Tinea pedis condition affects nearly one in four people worldwide. Despite this high prevalence, there have been no novel Rx or OTC innovations in multiple decades. "We wanted to create a treatment that wouldn't just fix the itch, but help people feel confident in their bare feet again," said Dr. Schanbacher.
Powerful Clinically Tested Results for Athlete's Foot Relief
In a recent clinical study, patients who used Dryello's dry stick formulation demonstrated strong efficacy:
90% of patients were cured of Athlete's Foot within 4 weeks*
89% reported less sweaty feet*
*Study: Clinical Study to Assess Tolnaftate 1% with a Novel Vehicle for the Treatment of Tinea Pedis, May 2025
Dryello is the first of many anti-infective products that comprise the Propedix pipeline. "Propedix and our R&D team have spent years developing the stick as a DryStik Technology Platform to create formulations and applicator technologies that enhance delivery of safe and effective existing anti-pathogenic agents," said Niv Caviar, CEO of Propedix. "The proprietary nature of our science, clinical results and supporting patents will help establish Propedix as a leader in novel dermatological treatments for skin disorders and antifungal infections."
About Athlete's Foot
Athlete's Foot is a highly contagious fungal skin infection that affects nearly 70% of the population at some point in their lives. It's often picked up in gyms, showers, locker rooms, and tight-fitting shoes. It thrives in warm, moist environments and frequently recurs even after treatment—making long-term solutions that combat both fungus and moisture essential. The global market for Athlete's Foot is estimated to be over $1B including both Rx, OTC and palliative therapies.
About Propedix
Propedix is a leading biopharma and consumer health company dedicated to advancing innovative treatments in topical dermatology and anti-infectives. Through a commitment to innovation, Propedix strives to provide effective, clinically tested solutions to fungal conditions. The Propedix team works diligently to expand the world of anti-fungal and anti-pathogen treatment through the use of their proprietary delivery and formulation technology. Propedix has established itself as a trusted name in the industry, centering around improving the quality of life for each patient.
Dryello™ is available now for purchase at dryello.com and on Amazon. Stick it to Athlete's Foot™
To learn more, visit propedix.com or dryello.com
Website:
SOURCE Propedix Inc.
WANT YOUR COMPANY'S NEWS FEATURED ON PRNEWSWIRE.COM?
440k+
Newsrooms &
Influencers
9k+
Digital Media
Outlets
270k+
Journalists
Opted In
GET STARTED
临床结果
100 项与 托萘酯 相关的药物交易
登录后查看更多信息
研发状态
10 条最早获批的记录, 后查看更多信息
登录
| 适应症 | 国家/地区 | 公司 | 日期 |
|---|---|---|---|
| 银屑病 | 日本 | 2007-03-22 | |
| 足癣 | 日本 | 2007-03-22 | |
| 花斑癣 | 日本 | 2007-03-22 |
登录后查看更多信息
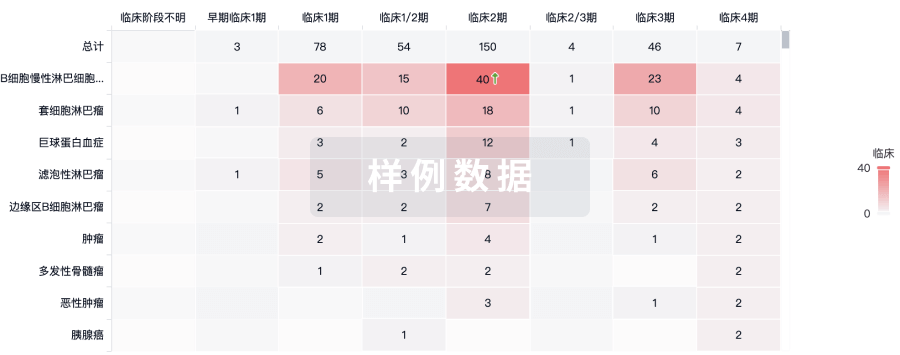
临床结果
临床结果
适应症
分期
评价
查看全部结果
| 研究 | 分期 | 人群特征 | 评价人数 | 分组 | 结果 | 评价 | 发布日期 |
|---|
No Data | |||||||
登录后查看更多信息
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
药物交易
使用我们的药物交易数据加速您的研究。
登录
或

核心专利
使用我们的核心专利数据促进您的研究。
登录
或
临床分析
紧跟全球注册中心的最新临床试验。
登录
或
批准
利用最新的监管批准信息加速您的研究。
登录
或

特殊审评
只需点击几下即可了解关键药物信息。
登录
或

生物医药百科问答
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用
