预约演示
更新于:2025-08-09
Selective PARP1 inhibitor(Acerand Therapeutics)
更新于:2025-08-09
概要
基本信息
非在研机构- |
权益机构- |
最高研发阶段临床前 |
首次获批日期- |
最高研发阶段(中国)- |
特殊审评- |
关联
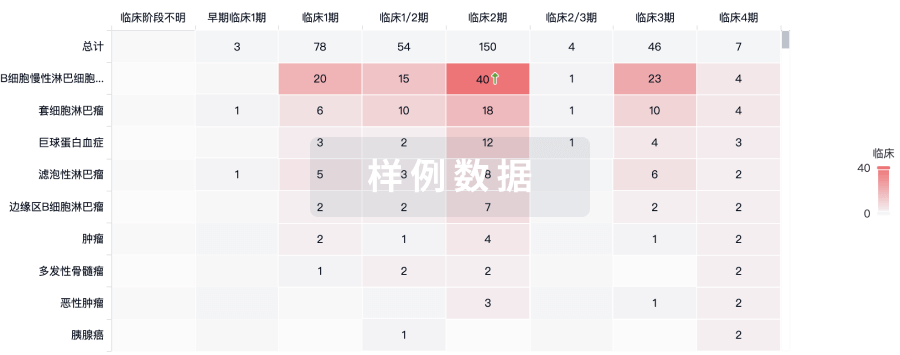
100 项与 Selective PARP1 inhibitor(Acerand Therapeutics) 相关的临床结果
登录后查看更多信息
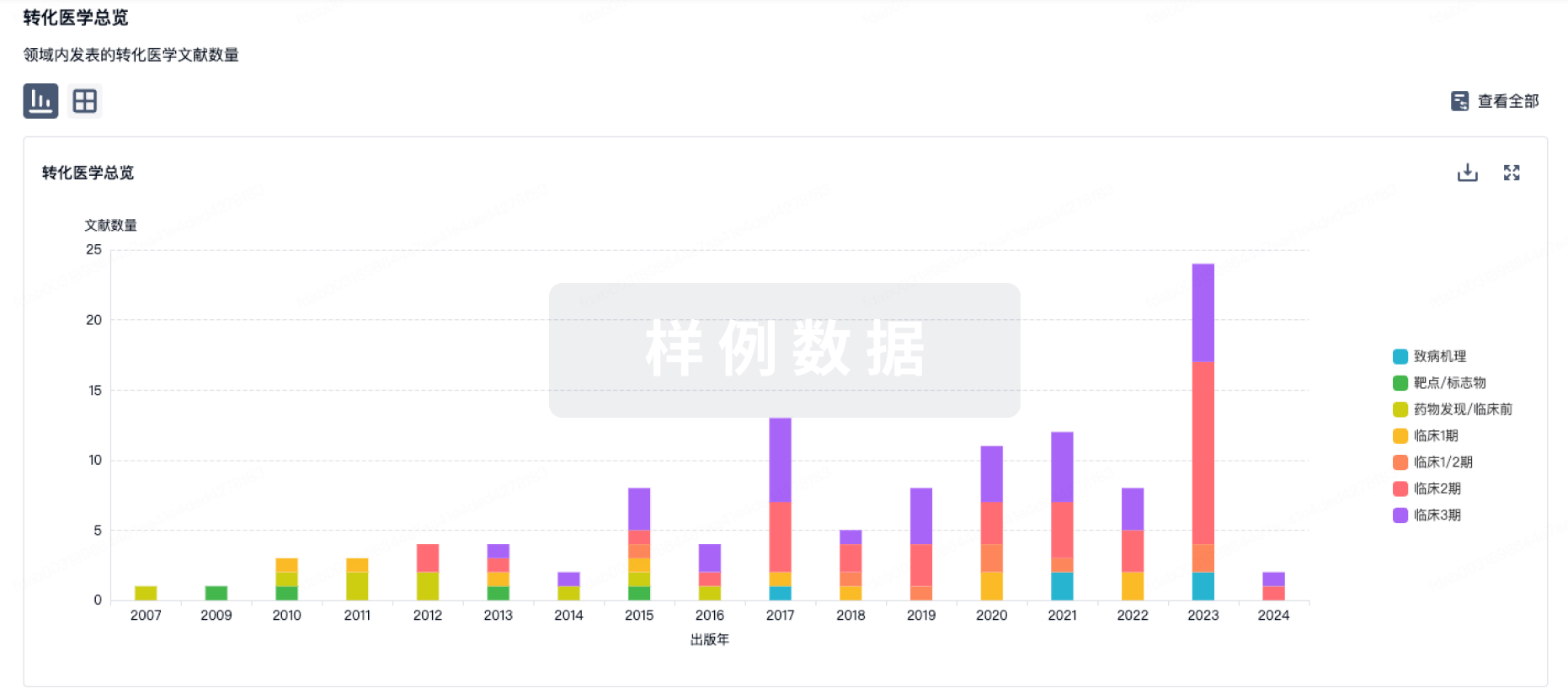
100 项与 Selective PARP1 inhibitor(Acerand Therapeutics) 相关的转化医学
登录后查看更多信息
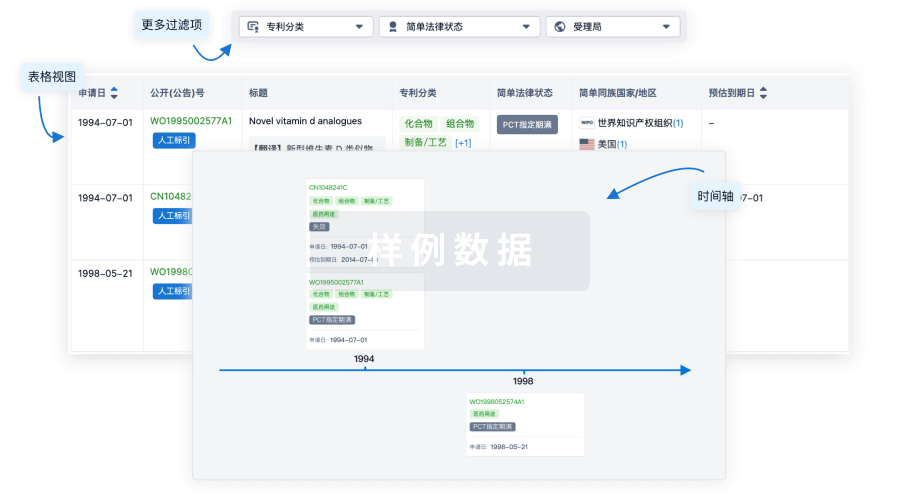
100 项与 Selective PARP1 inhibitor(Acerand Therapeutics) 相关的专利(医药)
登录后查看更多信息
6
项与 Selective PARP1 inhibitor(Acerand Therapeutics) 相关的文献(医药)2025-07-01·AMERICAN JOURNAL OF PATHOLOGY
Poly (ADP-Ribose) Polymerase 1 and 2 in B-Cell Lymphoma
Review
作者: Molina-Alvarez, Andrea ; Colomo, Luis ; Yélamos, José ; Sanchez-Gonzalez, Blanca
B-cell lymphomas represent a heterogeneous group of malignancies characterized by complex genetic, epigenetic, and microenvironmental alterations. Defects in the DNA damage response (DDR) are critical drivers of lymphomagenesis, generating therapeutic vulnerabilities that can be exploited by targeting key DDR regulators, such as poly (ADP-ribose) polymerase-1 (PARP-1) and PARP-2. Preclinical studies demonstrate that DDR-defective B-cell lymphomas are highly sensitive to PARP-1/PARP-2 inhibition, and early-phase clinical trials using nonselective PARP inhibitors, either as monotherapy or in combination with chemotherapy, immunotherapy, or epigenetic agents, have yielded encouraging results. However, emerging evidence reveals that PARP-1 and PARP-2 play distinct roles in B-cell lymphoma pathogenesis: loss of PARP-1 accelerates lymphomagenesis, whereas loss of PARP-2 delays tumor progression. These findings challenge the current paradigm of pan-PARP inhibition and highlight the need for isoform-selective strategies. Although PARP-1-selective inhibitors have entered clinical trials for homologous recombination-deficient tumors, the development of PARP-2-selective inhibitors remains at an early stage. Future research should prioritize the design of PARP-2-targeted therapies, coupled with biomarker-driven patient selection and rational combination strategies that enhance DNA damage and modulate the tumor immune microenvironment. Selectively targeting PARP-2 offers a promising approach to improving outcomes for patients with aggressive, refractory, or relapsed B-cell lymphomas and represents a critical step forward in advancing precision oncology within hematologic malignancies.
2023-03-27·Cancer research communications
The PARP1 Inhibitor AZD5305 Impairs Ovarian Adenocarcinoma Progression and Visceral Metastases in Patient-derived Xenografts Alone and in Combination with Carboplatin
Article
作者: Albertella, Mark R. ; Giavazzi, Raffaella ; Ghilardi, Carmen ; Leo, Elisabetta ; Formenti, Laura ; Bani, Maria Rosa ; Dellavedova, Giulia ; Staniszewska, Anna D. ; Decio, Alessandra ; Wilson, Joanne
Significance::
Selective PARP1i AZD5305 can exceed the efficacy of first-generation PARPi, which target both PARP1 and PARP2, and potentiates the efficacy of CPT when given in combination. AZD5305 alone or in combination with platinum delayed visceral metastasis, ultimately extending the lifespan of OC-PDX–bearing mice. These preclinical models mimic the progression of the disease occurring in patients after debulking surgery, and are translationally relevant.
2023-03-14·CLINICAL CANCER RESEARCH
Design and Preclinical Evaluation of a Novel B7-H4–Directed Antibody–Drug Conjugate, AZD8205, Alone and in Combination with the PARP1-Selective Inhibitor AZD5305
Communications
作者: Yuan, Jiaqi ; Vijayakrishnan, Balakumar ; Davies, Michael ; Wortmann, Philipp ; Howard, Philip W. ; Anderton, Judith ; Tosto, Frances Anne ; Rosenbaum, Anton I. ; Albertella, Mark R. ; Chesebrough, Jon ; Novick, Steven ; Wallez, Yann ; Tice, David A. ; Dimasi, Nazzareno ; Luheshi, Nadia ; McFarlane, Mary ; Sabol, Darrin ; Cooper, Zachary A. ; Masterson, Luke ; Leo, Elisabetta ; Dickinson, Niall J. ; Christie, R. James ; Cailleau, Thais ; Kinneer, Krista ; Huang, Yue ; Ball, Kathryn ; Wang, Jixin ; Monks, Noel ; Staniszewska, Anna D. ; Lewis, Arthur ; Sapra, Puja ; Hutchinson, Ian
Abstract:
Purpose::
We evaluated the activity of AZD8205, a B7-H4–directed antibody–drug conjugate (ADC) bearing a novel topoisomerase I inhibitor (TOP1i) payload, alone and in combination with the PARP1-selective inhibitor AZD5305, in preclinical models.
Experimental Design::
IHC and deep-learning–based image analysis algorithms were used to assess prevalence and intratumoral heterogeneity of B7-H4 expression in human tumors. Several TOP1i-ADCs, prepared with Val-Ala or Gly–Gly–Phe–Gly peptide linkers, with or without a PEG8 spacer, were compared in biophysical, in vivo efficacy, and rat toxicology studies. AZD8205 mechanism of action and efficacy studies were conducted in human cancer cell line and patient-derived xenograft (PDX) models.
Results::
Evaluation of IHC-staining density on a per-cell basis revealed a range of heterogeneous B7-H4 expression across patient tumors. This informed selection of bystander-capable Val-Ala–PEG8–TOP1i payload AZ14170133 and development of AZD8205, which demonstrated improved stability, efficacy, and safety compared with other linker–payload ADCs. In a study of 26 PDX tumors, single administration of 3.5 mg/kg AZD8205 provided a 69% overall response rate, according to modified RECIST criteria, which correlated with homologous recombination repair (HRR) deficiency (HRD) and elevated levels of B7-H4 in HRR-proficient models. Addition of AZD5305 sensitized very low B7-H4–expressing tumors to AZD8205 treatment, independent of HRD status and in models representing clinically relevant mechanisms of PARPi resistance.
Conclusions::
These data provide evidence for the potential utility of AZD8205 for treatment of B7-H4–expressing tumors and support the rationale for an ongoing phase 1 clinical study (NCT05123482).See related commentary by Pommier and Thomas, p. 991
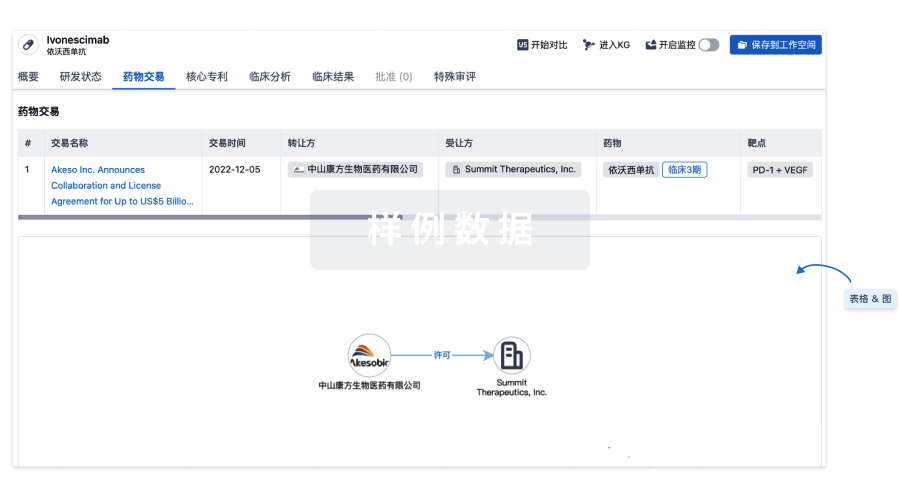
100 项与 Selective PARP1 inhibitor(Acerand Therapeutics) 相关的药物交易
登录后查看更多信息
研发状态
10 条进展最快的记录, 后查看更多信息
登录
| 适应症 | 最高研发状态 | 国家/地区 | 公司 | 日期 |
|---|---|---|---|---|
| 实体瘤 | 临床前 | 美国 | 2024-08-14 |
登录后查看更多信息
临床结果
临床结果
适应症
分期
评价
查看全部结果
| 研究 | 分期 | 人群特征 | 评价人数 | 分组 | 结果 | 评价 | 发布日期 |
|---|
No Data | |||||||
登录后查看更多信息
转化医学
使用我们的转化医学数据加速您的研究。
登录
或
药物交易
使用我们的药物交易数据加速您的研究。
登录
或
核心专利
使用我们的核心专利数据促进您的研究。
登录
或
临床分析
紧跟全球注册中心的最新临床试验。
登录
或
批准
利用最新的监管批准信息加速您的研究。
登录
或

特殊审评
只需点击几下即可了解关键药物信息。
登录
或

Eureka LS:
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用