预约演示
更新于:2025-05-07
Graying of Hair, Precocious
早熟性白发
更新于:2025-05-07
基本信息
别名 GRAYING OF HAIR, PRECOCIOUS、Graying of Hair, Precocious、WHITE HAIR, PREMATURE + [2] |
简介- |
关联
1
项与 早熟性白发 相关的药物靶点- |
作用机制- |
非在研适应症- |
最高研发阶段临床前 |
首次获批国家/地区- |
首次获批日期1800-01-20 |
5
项与 早熟性白发 相关的临床试验NCT06552039
Scientific Evaluation of the Safety and Efficacy of Herbal and Non Herbal Formulations in Mitigating Hair Fall, Promoting Hair Growth, and Preventing Premature Hair Graying.
This is proof-of-science, prospective, interventional, three-arm, double-blind, randomized, safety and efficacy real world evidence study of herbal and non herbal formulations in healthy human subjects having complaint of hair fall and pre-mature graying.
开始日期2024-08-24 |
申办/合作机构- |
ChiCTR2100047179
The safety and efficacy of concentration growth factor partly injection in white hair
开始日期2021-06-10 |
申办/合作机构- |
ChiCTR2000034710
A Randomized Controlled Clinical Study on Dumai 'Five Points' Pricking Therapy in the Treatment of Premature Hair Graying (Blood-Heat Type)
100 项与 早熟性白发 相关的临床结果
登录后查看更多信息
100 项与 早熟性白发 相关的转化医学
登录后查看更多信息
0 项与 早熟性白发 相关的专利(医药)
登录后查看更多信息
55
项与 早熟性白发 相关的文献(医药)2024-05-16·Boletín Médico del Hospital Infantil de México
Factores pronósticos del vitiligo en la edad pediátrica
Article
作者: Anda-Ortiz, Nabil De ; Morales-Sánchez, Martha A ; Villegas-Calzada, M Fernanda ; Acatitla-Acevedo, Graciela A
2024-05-09·Cureus
Fractal Pattern in the Premature Graying of Hair: A Case Report
Article
作者: Rashid, Rashid M ; Niazi, Maryam ; Kashyap, Alisha ; Black, Troy A ; Ali, Amna M ; Phan, Brandy
2024-03-22·Cureus
Multiple Behavioral Risk Factors As Assets for Chronic Disease Prevention: Observations From Urban Primary Care Settings in Crete, Greece
Article
作者: Smyrnakis, Emmanouil ; Volkos, Panagiotis ; Mantadaki, Aikaterini E ; Linardakis, Manolis ; Petraki, Chrysi ; Nioti, Kadiani ; Stachteas, Panagiotis ; Symvoulakis, Emmanouil K ; Karelis, Andreas ; Antoniou, Aikaterini M ; Mastronikolis, Stylianos
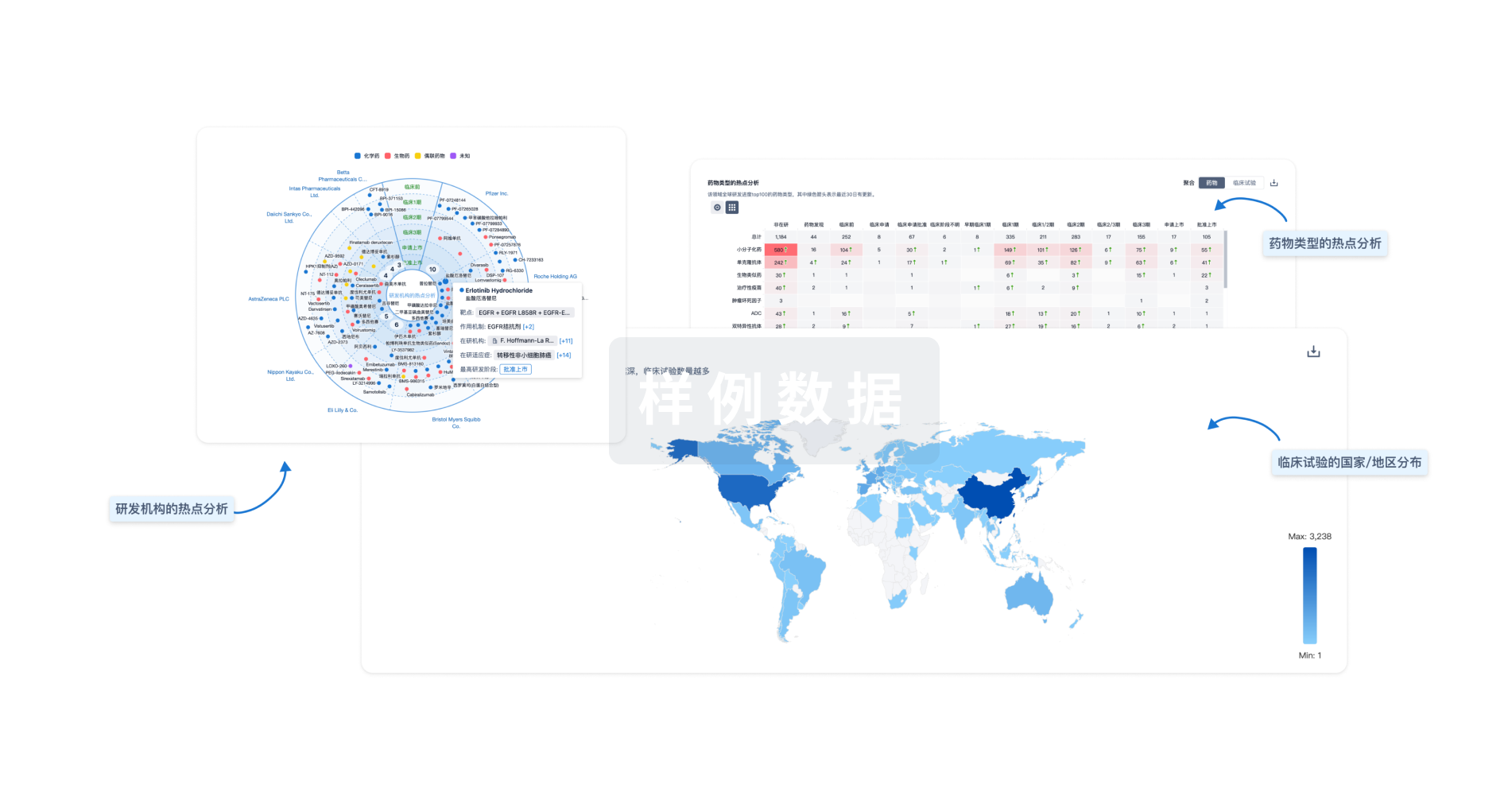
分析
对领域进行一次全面的分析。
登录
或
生物医药百科问答
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用

