预约演示
更新于:2025-05-07
Uterine Prolapse
子宫脱垂
更新于:2025-05-07
基本信息
别名 Descens uteri、Descensus uteri、Hernia, uterine + [45] |
简介 Downward displacement of the UTERUS. It is classified in various degrees: in the first degree the UTERINE CERVIX is within the vaginal orifice; in the second degree the cervix is outside the orifice; in the third degree the entire uterus is outside the orifice. |
关联
1
项与 子宫脱垂 相关的药物靶点- |
作用机制- |
在研机构 |
原研机构 |
非在研适应症- |
最高研发阶段批准上市 |
首次获批国家/地区 中国 |
首次获批日期2019-11-08 |
191
项与 子宫脱垂 相关的临床试验NL-OMON57159
The Influence of Pelvic floor muscle function on pessary Treatment success in patients with pelvic Organ Prolapse - TIPTOP study
开始日期2024-12-01 |
申办/合作机构- |
NCT06679621
A Telehealth Intervention to Increase Patient Preparedness for Surgery in Latinas
There are 3 aims of this study. In Aim 1 community patient partners will be enrolled to help guide the research being performed in all of the aims. Investigators will also administer a survey that will help determine factors associated with surgical preparedness. In Aim 2 investigators will develop an intervention to increase surgical preparedness using Human Centered Design Methods. Aim 3 will pilot test the intervention using mixed methods to determine feasibility and implementation outcomes.
开始日期2024-11-11 |
申办/合作机构 |
NCT06634459
The POMEGRANATE Trial: A Randomized Controlled Trial Comparing Pessary Home Management of Reia Pessary Versus Standard of Care Pessary for Treatment of Pelvic Organ Prolapse
This multi-centered, randomized controlled trial will evaluate the safety and efficacy of home use of the novel Reia System (RS), which includes the Reia pessary and applicator, compared to standard pessary care (Gellhorn or ring with/without support without knob) among women with stage II-IV pelvic organ prolapse (POP). A total of 182 participants will be recruited among pessary naïve patients who are symptomatic and choose a vaginal pessary for management of their POP from study sites specializing in Urogynecology and Reconstructive Pelvic Surgery (URPS). Participants will be assigned via 1:1 randomization using computer generated numbers in permutated groups of variable block sizes to either the intervention (the Reia System, RS) or standard pessary care (SPC) stratified by site. Participation in this trial will involve a total of four visits over six months. The primary outcome measure will be the number of successful self-managed pessary removal events completed over the six-month time frame. Secondary outcomes will include validated surveys to assess quality of life, adverse events and satisfaction with treatment.
Specific Aims
Aim 1: To compare number of self-management events over a 6-month period between subjects randomized to the Reia System and those randomized to standard of care pessary.
Aim 2: To assess successful fitting, number of refitting visits, and continued pessary use over a 6-month period between subjects randomized to the Reia System and those randomized to standard of care pessary.
Aim 3: To compare satisfaction with treatment and quality of life over a 6-month period between subjects randomized to the Reia System and those randomized to standard of care pessary.
Aim 4: To measure rates of adverse events and risk factors for adverse events over a 6-month period between subjects randomized to the Reia System and those randomized to standard of care pessary.
Specific Aims
Aim 1: To compare number of self-management events over a 6-month period between subjects randomized to the Reia System and those randomized to standard of care pessary.
Aim 2: To assess successful fitting, number of refitting visits, and continued pessary use over a 6-month period between subjects randomized to the Reia System and those randomized to standard of care pessary.
Aim 3: To compare satisfaction with treatment and quality of life over a 6-month period between subjects randomized to the Reia System and those randomized to standard of care pessary.
Aim 4: To measure rates of adverse events and risk factors for adverse events over a 6-month period between subjects randomized to the Reia System and those randomized to standard of care pessary.
开始日期2024-11-01 |
申办/合作机构 |
100 项与 子宫脱垂 相关的临床结果
登录后查看更多信息
100 项与 子宫脱垂 相关的转化医学
登录后查看更多信息
0 项与 子宫脱垂 相关的专利(医药)
登录后查看更多信息
8,614
项与 子宫脱垂 相关的文献(医药)2025-12-01·Techniques in Coloproctology
High and low take-off external prolapse phenotypes can be characterised preoperatively on defaecation proctography
Article
作者: Cunningham, C ; Singh, S ; Lindsey, I ; Cooper, E A ; Hodgkinson, J ; Yates, C
2025-12-01·Current Gastroenterology Reports
Rectal Prolapse in the Pediatric Population
Review
作者: Stratigis, John D ; Moon, James K ; Moon, James K. ; Stratigis, John D. ; Lipskar, Aaron M ; Lipskar, Aaron M.
2025-07-01·Biomaterials
Profiling of the macrophage response to polypropylene mesh burden in vivo
Article
作者: King, Gabrielle ; Therriault, Marrisa A ; Knight, Katrina ; Kottapalli, Srividya ; Artsen, Amanda ; Brown, Bryan N ; Meyn, Leslie ; Moalli, Pamela A
22
项与 子宫脱垂 相关的新闻(医药)2025-03-06
转自:中华中医药学会官微 编辑:水晶3月6日,中华中医药学会发布了《中药质量标志物研究技术指南》等6项团体标准公告。标准包含《中药质量标志物研究技术指南》、《中药复方非临床药理研究技术指南》、《含中药肠吸收液体外实验操作规程》、《常见中医症状-人类表型本体对照表》、《子宫脱垂中医诊疗指南》、《子痫前期中医诊疗指南》。
为推进中医药标准化建设,制定满足市场和创新需求的团体标准,加快中医药标准化发展进程,中华中医药学会标准化办公室组织了团体标准发布审查,专家对《中药质量标志物研究技术指南》等6项团体标准的科学性、实用性进行论证,经过专家审查同意该团体标准发布,且公示期间无异议。经中华中医药学会秘书长办公会审议,现予以公告。
《中药质量标志物研究技术指南》简介
《中药质量标志物研究技术指南》由天津药物研究院有限公司刘昌孝院士牵头,张铁军研究员组织全国50位专家共同参与制定。本指南意在明确质量标志物发现和确定的原则、研究路径、技术方法,以及基于质量标志物的中药质量评价方法和质量标准研究,构建中药质量标志物研究的科学模式,促进中药全程质量溯源体系建设和产业监管发展。本指南于2022年7月由中华中医药学会立项,研制程序和方法按中华中医药学会《中华中医药学会团体标准管理办法》等要求执行。本指南制定集合了起草单位各团队中药质量标志物研究工作,并结合公开发表的中药质量标志物文献调研结果,经过多个学科专家充分讨论后形成共识,同时广泛征求来自大专院校、科研院所、检验检测机构及中药生产企业的多学科专家意见,保证了指南的实用性、规范性、科学性及可行性。(此部分内容由项目组提供)
《中药复方非临床药理研究技术指南》简介
本技术指南旨在强化对中药复方药理学基础研究、中药复方新药研发等应用的指导作用。在基础研究时,对供试样品的基本信息提出要求,旨在明确其物质基础,保障其质量稳定可重复,提出从直接作用、间接作用、辅助作用三条作用途径形成中药复方有效性完整的证据链体系,充分展示“多成分、多途径、多靶点”整体作用特点,形成中药复方作用机制研究的基本模式,拓宽中药复方药理学研究深度和广度。在中药复方新药研发时,明确中药复方非临床药理学对不同中药新药研发情形的作用及意义,为中药复方临床实验方案设计和疗效指标选择提供参考;对中药复方新药的关键信息进行对比研究,为源于基础研究或缺乏人用经验的中药复方新药早期立项提供重要支持;此外,说清楚讲明白中药复方新药的药效物质基础及作用机理,为优先审评审批等情形提供参考,促进基础与临床之间的相互转化研究。本技术指南紧跟科技前沿,以中药整合药理学为指导,通过整体与局部、宏观与微观、药代与药效之间的整合研究,实现从全景式描述到精准机制研究、从多维“PK-PD”定性到关键成分的“PK-PD”定量研究,体现系统论与还原论间的统一。同时,强调在拟临床思路的指导下,以临床价值为导向,动物模型需与临床疾病在病理生理等方面具有相似性,构建与临床相关联的多层级、多维度药效学的指标体系,开展不同维度、不同层级指标之间关联性研究,实现基础研究与临床研究成果之间的相互转化,保障中药复方药理学在动物模型可稳定可重复、药效评价可量化、作用机制可解释等。(此部分内容由项目组提供)
《含中药肠吸收液体外实验操作规程》简介
目前中药体外药理研究方法主要为直接加药法和含药血清法,但两种研究方法带来的杂质均会干扰实验结果的准确性。肠吸收液最初是体外肠道吸收的生物模型,广泛用于药物的吸收及代谢等研究。本项目负责人杨洪军研究员长期致力于含中药肠吸收液的体外药理研究,利用外翻肠囊法制备含中药肠吸收液,以肠吸收液为药物载体,将其应用于中药及复方体外药理活性评价、分子机制解析、有效成分辨识和质量评价等研究,积累了大量的研究工作基础。
本技术指南建立用于体外实验研究的含中药肠吸收液制备标准操作规程,对制备含中药肠吸收液的相关技术要素如实验动物、试剂材料、仪器设备、操作步骤、操作注意事项、体外实验样品处理以及质量保证和控制等技术要素进行详细的规范,使其可应用于细胞、离体组织器官和类器官等体外实验,开展药效评价、机制研究和有效成分辨识等体外药理研究,使后续的实验研究结果具有科学性、正确性和可重复性,提高中药及复方体外药理实验的可信度及效率。(此部分内容由项目组提供)
《常见中医症状-人类表型本体对照表》简介
中医症状的标准化和规范化是一项基础性、战略性、全局性工作,是推动中医药国际化发展的必由之路。然而由于理论基础、思维模式、概念内涵、表述方式等不同,中医症状术语与现代医学难以汇通和对应,阻碍了中医症状的标准化、规范化研究与转化应用。人类表型本体数据库(Human Phenotype Ontology,HPO,https://hpo.jax.org/)是一个用于标准化描述人类疾病表型异常的数据库,通过建立标准化医学名词和术语,精准描述患者症状表型,促进疾病诊断,确定致病基因,寻找疾病与特定表型间联系。鉴于此,起草团队以规范化和标准化的常用症状为切入点,建立中医症状与人类表型本体(HPO)表型之间映射关系。
本标准从国家标准《中医药学名词》(2004)、《中医药学名词》(外科学皮肤科学肛肠科学眼科学耳鼻喉科学骨伤科学)(2013)、《中医临床基本症状信息分类与代码》(T/CIATCM 020-2019)、《中医症状鉴别诊断学》(第二版2000)等收集中医症状,对同义词进行标准化处理。基于ETCM 2.0数据库(http://www.tcmip.cn/ETCM2/front/#/)收录的古代方剂及中成药所治疗的中医症状进行频次统计,以此界定常见症状。并依据《中医诊断学》对上述中医症状进行四诊信息分类。最后,基于HPO人类表型本体数据库进行检索和匹配,按照中医症状-HPO对应性评价原则,建立强、中、弱三级对应性评价等级,构建本指南。
本标准从症状角度出发,建立常见中医症状-人类表型本体(HPO)对照表,将根据需要进行不定期更新。本标准将有利于促进中医从传统诊疗模式(望、闻、问、切)与现代分子诊疗模式(基因测序等)相结合,以大数据、人工智能、系统生物学等新兴学科促进中医表型组学的发展,为中医证候科学内涵、方药作用机制的深入研究提供有效途径,为实现中医药精准医疗、中西医语言互通、中医药国际化和现代化发展奠定基础。(此部分内容由项目组提供)
《子宫脱垂中医诊疗指南》简介
子宫脱垂作为临床常见的盆底功能障碍性疾病,严重威胁女性的身心健康和生活质量。中医药治疗子宫脱垂历史悠久,可有效改善临床症状。《中医妇科常见病诊疗指南-子宫脱垂(ZYYXH/T235-2012》首发于2012年,对本病的中医临床诊疗发挥了重要作用,但原指南发布已逾十年,目前对子宫脱垂的辨证、诊疗成果层出不穷。基于此,遵照循证医学的原则,以文献检索为前提,整合近10余年中医药治疗子宫脱垂的研究成果,采用问卷调查、专家论证、证据评价等多种形式,对原指南病因病机、诊断要点、鉴别诊断、辨证分型、中成药及非药物疗法等方面进行了修订,制定出科学、规范、能切实指导临床的诊疗指南,以期进一步提高子宫脱垂诊治率,改善妇女的生活质量。(此部分内容由项目组提供)
《子痫前期中医诊疗指南》简介
子痫前期(Preeclampsia,PE)是造成孕妇严重妊娠期合并症和不良妊娠结局的重要原因之一,常在孕20周后出现新发高血压和蛋白尿,或在无蛋白尿时合并血小板减少、肝肾功能不全等其他相关症状及体征。PE具有病情危急,进展迅速的特点,不仅给患者及其家庭带来严重的经济负担,而且严重威胁着患者的身心健康。中医药治疗PE积累了大量的临床经验与临床试验研究成果,运用四诊合参,辨证论治,临床疗效较好。同时中医“治未病”未病先防、已病防变、已变防渐理论在PE早期识别与防范中发挥着重要的作用。为进一步规范PE的中医诊疗,促进中医诊治PE水平的提高,项目组根据《世界卫生组织指南制定手册》的指南制定流程、中华中医药学会团体标准管理办法以及GRADE系列文章的方法学等相关要求,遵循“循证为主、共识为辅、经验为鉴”推荐原则,制定了《子痫前期中医诊疗指南》。(此部分内容由项目组提供)
(标准全文请到“全国团体标准信息平台”检索查看)
推荐阅读:
蒲公英Ouryao视频号
投稿、广告、商务合作:
Qinrenlvcha
2024-11-18
MONDAY, Nov. 18, 2024 -- It’s possible to correct a woman’s pelvic prolapse using her own muscle tissue in robot-assisted surgery, a new study demonstrates.
In the procedure, tendon muscle is transferred from the thigh to the uterus or cervix, repairing a pelvic floor that’s become weakened and is allowing organs to press into each other, researchers explained.
The newly developed procedure successfully corrected prolapse in the first 10 female patients, the team reported Nov. 12 in the
International Urogynecology Journal
.
"This pilot study shows excellent clinical outcomes, with an improved quality of life for the patients," said senior researcher
Dr. Dominique Konsgen-Mustea
, head of urogyenecology at University Hospital Bonn in Germany.
With pelvic prolapse, the pelvic floor muscles weaken to the point that one or more organs -- the bladder, uterus, urethra or rectum -- start pressing into the vagina. Symptoms can include difficult urination, urinary tract infections, painful sex and constipation.
Pelvic prolapse typically occurs after pregnancy and childbirth, researchers said in background notes. Aging, excess weight and conditions that cause frequent coughing also increase a woman’s risk of pelvic prolapse.
Surgery can correct a prolapse, typically by implanting a synthetic mesh fabric that reinforces the pelvic floor, researchers said.
But using a person’s own muscle, taken from elsewhere in the body, could work even better than the synthetic mesh, doctors reasoned.
In the new procedure, researchers make a small incision in the back of the knee and remove part of the thigh tendon. The tendon is then implanted into the pelvic floor.
"The advantage of this method is that no foreign material enters the body," Konsgen-Mustea said in a university news release. "And removing the tendon also has no negative effects on the leg: it remains pain-free and, in the long term, unrestricted in terms of mobility."
Doctors performed the first robot-assisted pelvic prolapse surgery in June 2022, and had carried out the first 10 by February 2023, researchers said.
All 10 patients had positive outcomes a year after their surgery, researchers said. None suffered another prolapse, and there were no complications from the surgery.
"With the DaVinci robot, we have a highly magnified 3D-image and can therefore perform the surgery very precisely,” Konsgen-Mustea said. “This makes the procedure tissue-sparing and bleeding-less, and we can easily reach all deep compartments of the pelvic floor.”
Whatever your topic of interest,
subscribe to our newsletters
to get the best of Drugs.com in your inbox.
2024-10-15
·梅斯医学
病人进了手术室,医生却索要3000元“专家费”不给不做手术?卫健委回应
医生索要“专家费”这个事已经过去了好几天,但该事件带来的深刻讨论远没有结束,我们需要一个明确的指导。
先来回顾一下事件。
10月10日,四川广元一名网友发视频爆料称:我母亲在广元市中医院做手术时,该院心血管内科的安医生向家属索要了3000元现金红包,不给就不做手术。
据爆料人徐先生描述,9月3日凌晨,其母亲出现呕吐、肚子疼等症状,随后紧急送往广元市中医院急诊科,诊断为因感染出现严重脱水,当即住院治疗。治疗9天后,医院通知可办理出院手续,在其准备办理出院时,患者出现心跳加速的症状,医生表示心脏有问题,必须立即手术。
徐先生说道:“事发太突然,我和家人来不及询问究竟是什么病,母亲已被护士推进了手术室。手术前,我和父亲被叫到一间医生办公室,安医生要求我们准备3000元现金,是额外的,我要求手机转账,安医生说必须是现金,不能转账。”
为确保手术顺利,徐先生的父亲随后给了安医生3000元现金。爆料的视频清晰记录了安医生收取现金和清点现金的全过程,在确认是3000元后,装进了白大褂口袋。收取现金后,患者手术顺利进行,术后3天出院。
9月18日,徐先生给母亲办了出院手续,事后越想越气。他说道:“我就不明白,这3000元是什么费用?当时医生也没有告知我们,电子票据上显示,母亲住院费用合计80596元,3000元没有列入其中。”
10月10日上午,为了搞清楚3000元的用途,徐先生拨打了安医生的电话。安医生在电话中称,徐母住院时心脏不好,在病情稳定后需要做心脏射频消融术,收取的3000元是专家费,不是红包。随后安医生在电话中骂徐先生“你这人怎么这样,你是有神经病吧”。
在这次通话不久,一名自称广元市中医院领导的男子给徐先生打电话称,医院会处理此事,也会给他一个答复。
下午,该医院工作人员向徐先生提出,“可以退还3000元,但删掉视频。”徐先生未答应。
舆论发酵后,广元市卫生健康委员会工作人员进行了回应,表示会向广元市中医院核实此事,并详细调查事情缘由,如果属实,会对医生进行相应处理。
据了解,广元市中医院是广元市唯一集医疗、教学、科研于一体的国家三级甲等中医医院,涉事的心血管内科安医生为副主任医师,2020年驰援湖北武汉为抗疫做出过贡献。这3000元到底是不是飞刀费?如果是合乎规定的飞刀费,不应被指责卫健局曾认定收取飞刀费无过错!
这一事件引发了极其广泛的关注和讨论,人们首先困惑的就是医生为什么会要这3000元专家费?专家费到底是什么意思?要把钱给谁?
四川广元当地一名网友表示:“大家不要再多想了,我清楚得很,所谓的专家费就是飞刀费,钱是给请来的专家的。如果是大城市很好的专家请过来做手术,那3000元真的很便宜了,飞刀也是被允许的。如果没有请大医院的专家,那就不能收飞刀费。现在要查的是,给这个患者做手术的专家到底是不是请来的!”
成都一名自媒体大咖直言不讳地说道:“人心难测呀!所谓的红包,就是外请专家的费用,这个费用,大夫肯定和患者家属提前沟通过,具体要多少钱也都讲明白了。这名患者家属当时肯定已经答应了,所以不存在什么‘母亲躺手术室,医生逼要专家费,不给不做手术’的情况。”
“人心险恶呀,既要享受专家手术,又不想出钱。你要是不愿意让专家做手术,就别答应,把机会让给其他人,或者你觉得贵,可以出院去上级医院自己住院。但是,你既然答应了,专家都来了,又搞这一套!你一人耍赖,恐怕要断了以后这个医院外请专家的路,受害的是整个广元的群众!”
江苏一名网友则表示:“我们现在需要医院明确告诉我们这3000元是不是飞刀费!如果是飞刀费,那就没问题,并且我们还会帮着医院谴责这名不诚实、想占便宜的患者家属,并勒令他向医院、向安医生赔礼道歉,并恳请某音等平台封掉这个家属的账号,因为他涉嫌造谣诋毁。因为飞刀很常见,在飞刀之前,医患双方都是知情并同意的,在小医院看病,我们巴不得大专家过来给我们做手术呢。如果这不是飞刀费,医院没有请外来的专家过来,当事医生竟然众目睽睽之下索要现金红包,那这就是犯罪、违反医德医风,就请卫健部门狠狠地、顶格处罚这名医生!”
这件事的逻辑一下子清晰了,正如江苏这名网友所说的,这3000元到底是不是飞刀费?如果是飞刀费,在双方知情同意、合乎规定的情况下,这名网友做出此种姿态,是不诚实、不守信、破坏规则的行为,理应向当事医生和医院道歉,并受到网友谴责!如果这3000元不是飞刀费,而是实打实的、见不得光的、没有任何依据的红包,又或者患者事先对飞刀并不知情,医生没有解释,单方面开展飞刀,那医生就应该受到最严格的惩处。
事实上,涉及到飞刀,只要合乎规定,我们一般都是支持的。
2024年01月17日,郑州疾控中心就发表了一篇题为《飞刀手术缘何屡被投诉?如何破解飞刀难题?》,其中表明了自己的态度。
郑州疾控中心表示,此前报道,河北李先生投诉某县级医院,称“其母亲因子宫脱垂住院,手术麻醉后,医生要求其现金支付13000元专家费。”
医院回应表示:这次手术是外聘专家(即“飞刀”医生)进行的,收费合规,并且明确告知该费用是直接以现金的方式给专家,不能报销,不通过医院,患方表示同意。
随后,当地卫健局调查后认定:医院不存在过错行为,合法合规!
在评论医生“飞刀”时,郑州疾控中心就在文中表示:“目前,社会和医疗界大多认为医生飞刀现象是患者、医院、医生三方共赢的局面,但这个看似一举三得的方案,却屡屡成为医患矛盾的催化剂和医疗事故的导火索。如何破解这一难题?依法执业是关键!”近3成医生飞刀过,说不清的飞刀,未来我们该如何面对?
飞刀,离我们医生太近了,凡是大三甲的专家,都可能接触过飞刀。
在一项针对3000多名医生参与的调查中,55%的医生称所在医院的医生飞刀现象普遍,近三成医生表示自己曾经飞刀过。
其实,医生“飞刀”的情况建国以来发生过多次变化。
在《中华人民共和国执业医师法》尚未实施之前,代表医生职业身份的只有职称和医师资格证,没有执业证,更没有对执业地点的限制。也就是说,医生在哪里都可以执业,那是医生们“飞刀走穴”最自由的时期。
1999年,情况变了,新施行的《执业医师法》确立了我国医师的注册制度,它将医生与公立医院紧紧地捆绑在了一起,医生只有通过国家统一考试,才能获取执业资格,无法自由选择行医的机构,只能在一家医疗机构注册,否则就是非法行医。
在《执业医师法》出台前,医院对待医生外出飞刀的态度,总体以支持为主。《执业医师法》出台后,“飞刀走穴”正式成为了非法执业行为,院长的态度也发生了微妙的变化,一般都不支持。
这是因为《执业医师法》规定,医师必须在注册的执业地点执业,医生若去其它医院会诊、做手术,必须要拿到会诊单。如果医生私自“飞刀走穴”,不出现意外倒还好,一旦产生医疗责任,则由医师所在的医院承担,于是院长们变得非常谨慎。
随着中国加入WTO,经济飞速发展,不同地区的医疗资源也出现了不平衡,民众开始极度渴望大医院的专家飞刀进入小医院,呼声很高。
于是,情况又变了。2009年,新一轮医改正式启动,医改方案中,探索“注册医师多点执业”在社会各界引起广泛关注。这是一个重要的时间节点,医师“多点执业”政策一度被不少人认为是“飞刀走穴”问题的解决方案。
2017年,《医师执业注册管理办法》出台,其中规定,医生在其他医疗机构执业,只需备案即可,再也不需要获得原单位的批准。此后,卫健委又多次发文支持“多点执业”,鼓励“医生兼职”。
到2019年,全国范围内注册多点执业的医师为11万,医生飞刀也越来越普遍,越来越阳光化,各级行政管理机构正试图将“飞刀走穴”纳入行政管理体制。
尽管飞刀已经很普遍,社会和民众需要飞刀,也接纳了医生飞刀,但是迄今为止,没有任何一个官方文件能明确表示“飞刀”这种行为是合规的还是不合规的,它有点说不清。
现如今,在大医院一床难求、名医一号难得的情况下,飞刀是普通人接触到顶级专家最简单的方式。
对于患者来说,不用人生路不熟地跑到外地排队等病床,不用抢号、挂号、重复检查,更重要的是,患者在自家门口就能得到更好的治疗,实在省钱、省心、省力;对于医生来说,飞刀去外地,既治了病、救了人,又在经济上获得了一定报酬,只要精力和时间允许,这完全就是一种兼职,可以尝试;对于医院来说,专家过来手术,既提高了技术和水平,收获了患者满意度,拓展了品牌和影响力,又完成了“大病不出县”的分级诊疗任务,何乐而不为呢?对于医保来说,因专家高质量的手术减少了患者并发症,提高了治疗效果,总体上减少了病人医疗费用报销的支出,也最终获益。
可以说,飞刀是一件多方获益的好事,但由于需要患者额外出钱,不能报销,总让患者觉得这是“红包”、是医生的“灰色收入”。
其实,医生飞刀是实实在在的兼职,医患双方互相知情,心甘情愿为之买单,飞刀费本质上是非常阳光的。
总之,飞刀现象是医疗资源分布不均的产物,需要在法治的轨道上规范运行。只有为飞刀正名,使飞刀阳光化,摆脱污名化,飞刀如今面临的困境才能减少,优质的医疗资源才能共享,各方人士才能共赢。
撰文 | 阿拉斯加宝
编辑 | 阿拉斯加宝
●Nature重磅:饭吃“六分饱”和间歇性禁食能延寿,但是要付出代价的!谷歌旗下抗衰老研究公司最新发文
●哀悼!近期两名顶级科主任突然离世!享年均为59岁!15岁考上大学、天才医生、风湿免疫专家、糖尿病防治大咖!我们无比惋惜悲痛
●每一口外卖、瓶装水都影响生殖健康!柳叶刀子刊:微塑料恐侵入并损伤男性生殖系统,尤其是不粘锅涂层
版权说明:梅斯医学(MedSci)是国内领先的医学科研与学术服务平台,致力于医疗质量的改进,为临床实践提供智慧、精准的决策支持,让医生与患者受益。欢迎个人转发至朋友圈,谢绝媒体或机构未经授权以任何形式转载至其他平台。
点击下方「阅读原文」 立刻下载梅斯医学APP!
分析
对领域进行一次全面的分析。
登录
或
生物医药百科问答
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
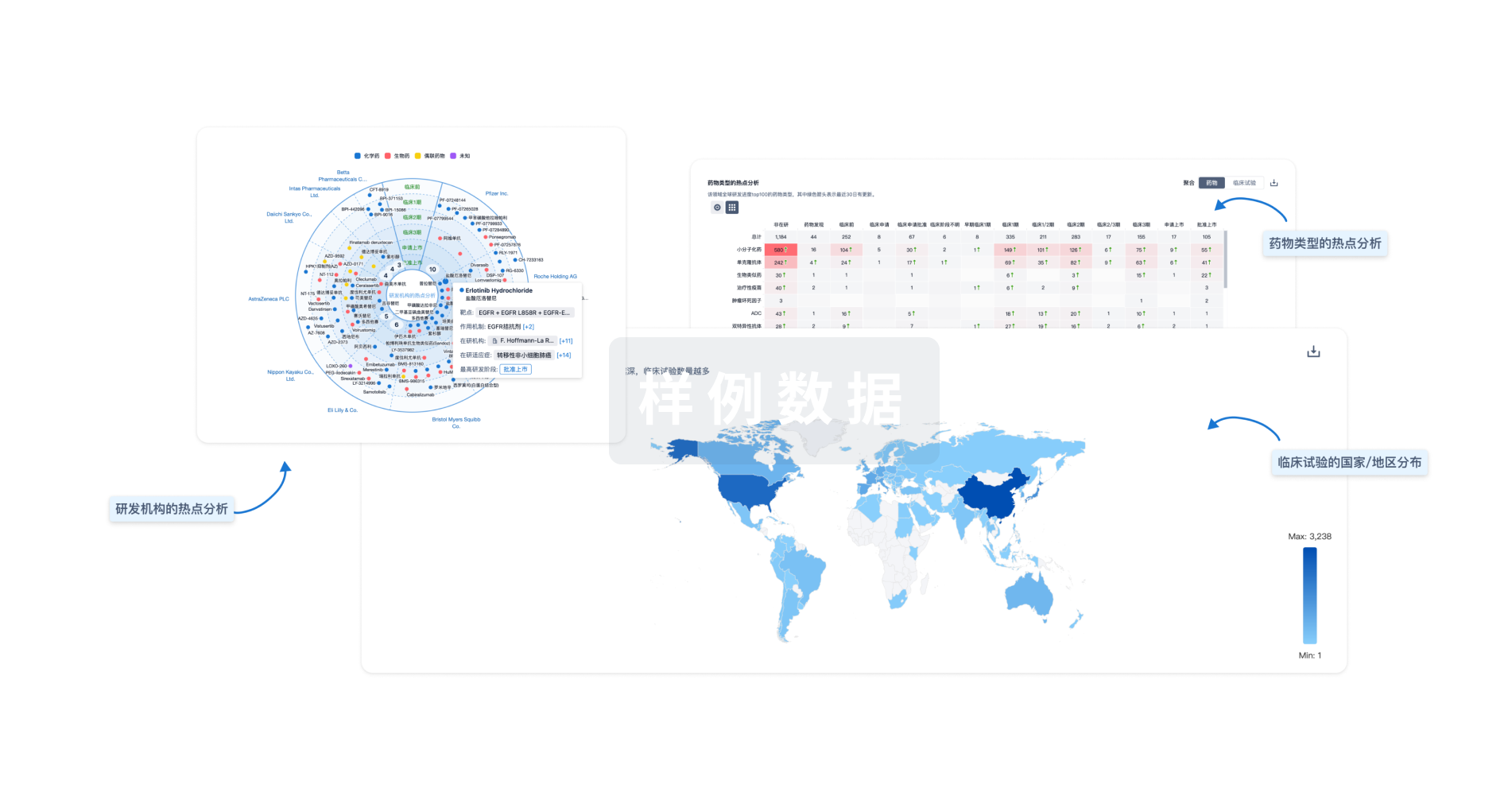
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用

